Yeast infections: what to watch for and how to get relief
Got itching, burning, or unusual discharge? Those are the common signs of a yeast infection, most often caused by Candida. It’s annoying and uncomfortable, but many cases are treatable at home with simple steps. This page gives quick, practical info so you can decide what to try first and when you need a clinician.
Quick symptoms & causes
Typical symptoms include strong itching, soreness, a thick white discharge (often described like cottage cheese), burning during urination or sex, and redness or swelling of the affected area. Men can get yeast infections too—look for redness, itchiness, or a rash on the penis.
Common triggers: recent antibiotics, high blood sugar (diabetes), hormone changes (pregnancy or birth control), tight or synthetic clothing, and a weakened immune system. Swimming pools, douches, or perfumed soaps can also upset the local balance and invite yeast growth.
Treatment, home care, and when to see a doctor
Over-the-counter antifungal creams and suppositories with miconazole or clotrimazole work well for many vaginal yeast infections. For stubborn or recurrent cases, doctors often prescribe a single oral dose of fluconazole (commonly 150 mg) or a multi-day regimen. Don’t mix treatments without asking a clinician—some medicines don’t help every type of fungus.
For skin yeast infections (like under breasts or in groin folds), keeping the area dry and wearing loose cotton can speed healing. Antifungal powders and topical azole creams usually clear these infections in a week or two.
Simple home tips: wear breathable cotton underwear, avoid tight pants, skip scented soaps and douches, and change out of wet swimsuits quickly. If you have diabetes, keeping blood sugar under control lowers recurrence risk. Probiotics may help some people, but evidence is mixed—think of them as a low-risk add-on, not a cure.
See a doctor right away if you have a fever, severe pain, unusual bleeding, or if symptoms don’t improve after treatment. Also consult your provider if you get four or more yeast infections a year—recurrent infections need a different approach and testing to rule out other causes.
If you’re unsure whether it’s a yeast infection or another problem (like bacterial vaginosis or a sexually transmitted infection), get tested. Accurate diagnosis avoids wasted treatments and gets you the right medicine faster.
Want detailed drug info? Our Lamisil guide explains terbinafine (useful for some skin and nail fungi), while other articles cover antifungal safety and buying meds online. Read those if you need deeper, practical help on specific drugs and where to find them safely.
Short, practical plan: spot the symptoms, try an OTC azole for uncomplicated cases, follow up with your clinician if things don’t improve or if symptoms are severe or recurrent. That approach usually gets you back to normal fast.
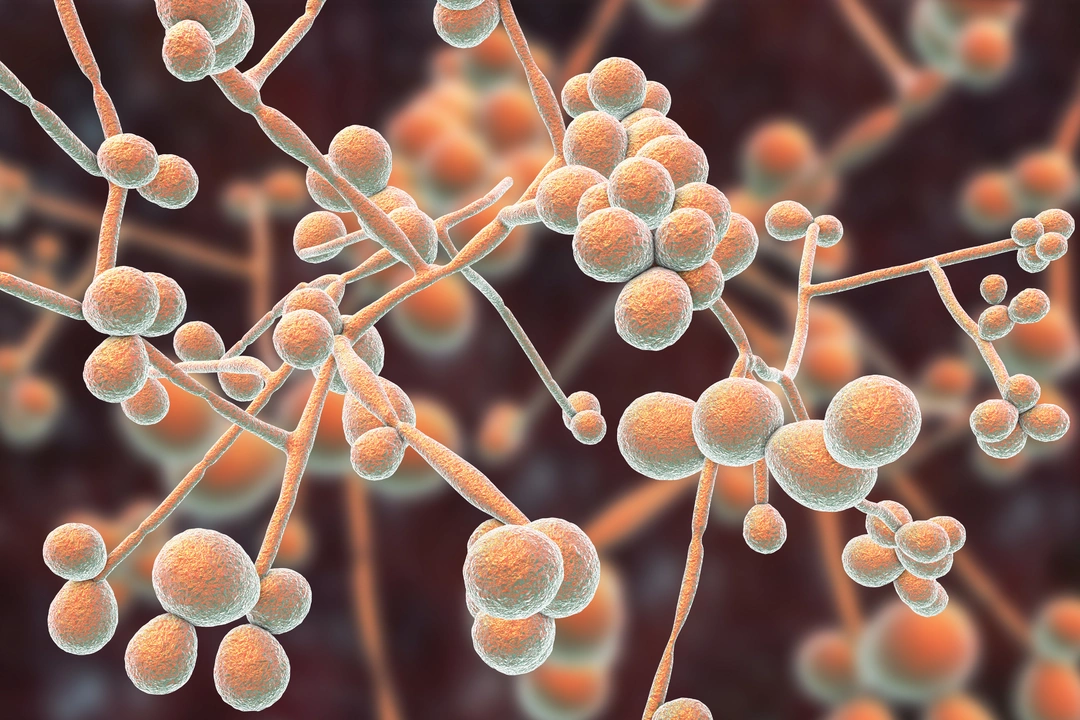
The Science Behind Yeast Infections of the Skin: What's Happening Under the Surface
As a blogger, I recently delved into the fascinating world of yeast infections of the skin. I discovered that these infections are caused by an overgrowth of yeast, usually of the Candida species, which normally live harmlessly on our skin. However, when conditions like warmth, moisture or a weakened immune system create an imbalance, these yeast can multiply and cause uncomfortable symptoms like itching, redness, and even a rash. It's interesting to learn that our body's natural defenses usually keep these infections at bay, but sometimes they need a little help from antifungal medications. Overall, understanding the science behind yeast infections not only satisfies our curiosity but also helps us to manage and prevent these annoying skin conditions.
Read More




