Understanding Yeast Infections of the Skin
When we think of yeast infections, we usually imagine the uncomfortable and embarrassing symptoms associated with vaginal yeast infections. However, yeast infections can also occur on the skin, causing various symptoms and complications. In this article, we'll delve into the science behind yeast infections of the skin and explore what's happening under the surface.
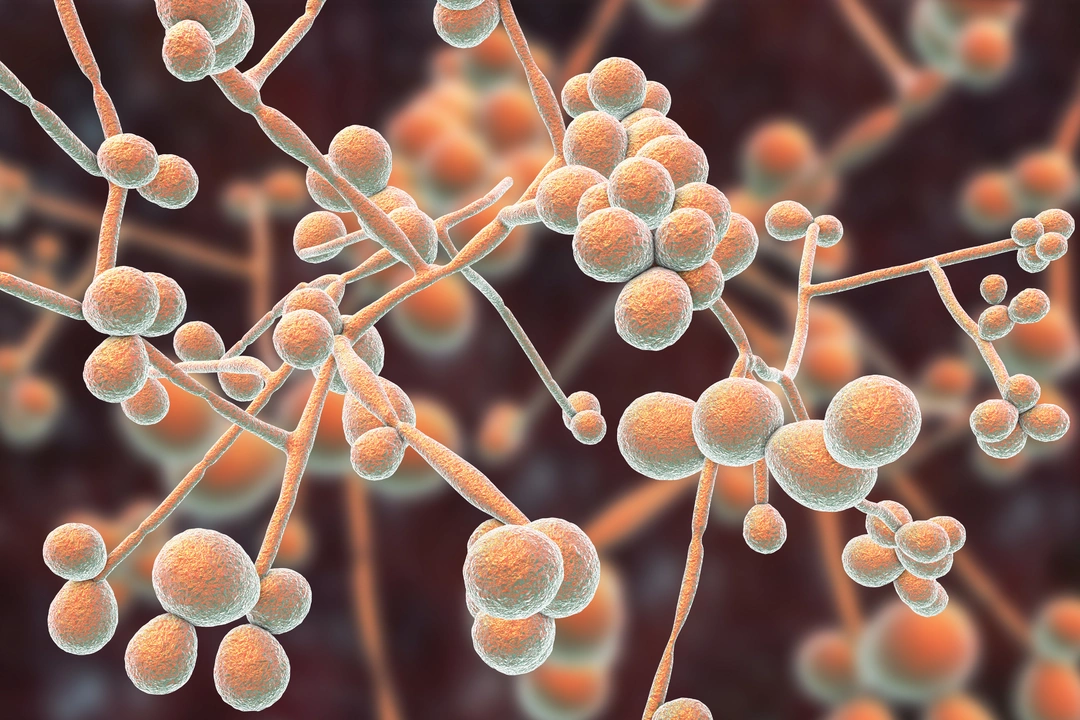
The Role of Yeast in Our Bodies
Yeast is a type of fungus that lives on the skin and inside the body. In small amounts, yeast is harmless and even necessary for our overall health. Yeast helps with digestion and nutrient absorption, as well as playing a role in maintaining the balance of bacteria in our bodies. However, when the balance of yeast and bacteria is disrupted, a yeast infection can occur. This can happen on the skin or in other areas of the body, such as the mouth, throat, or genitals.
Causes of Yeast Infections of the Skin
There are several factors that can contribute to the development of a yeast infection on the skin. These include:
- Moisture and humidity, which create an ideal environment for yeast growth
- Friction and irritation, such as from tight clothing or frequent rubbing
- Use of antibiotics, which can disrupt the balance of bacteria and allow yeast to overgrow
- Weak immune system, which can make it harder for the body to fight off infections
- Diabetes or other conditions that affect blood sugar levels, as yeast feeds on sugar
By understanding the factors that can contribute to a yeast infection, we can take steps to prevent them from occurring.
Symptoms of Yeast Infections of the Skin
Yeast infections of the skin can cause a variety of symptoms, including:
- Redness and inflammation
- Itching and burning sensations
- Cracked, scaly, or peeling skin
- Pustules or blisters
- Swelling and tenderness
These symptoms can be uncomfortable and may worsen if left untreated. It's essential to recognize the signs of a yeast infection and seek medical advice for proper diagnosis and treatment.
Diagnosing Yeast Infections of the Skin
If you suspect you have a yeast infection of the skin, it's essential to consult a healthcare professional for an accurate diagnosis. Your doctor will examine the affected area and may take a skin scraping to be analyzed under a microscope. This will help determine if yeast is the cause of your symptoms and rule out other skin conditions, such as eczema, psoriasis, or dermatitis.
Treatment Options for Yeast Infections of the Skin
Once diagnosed, your healthcare professional will recommend an appropriate treatment plan to address your yeast infection. This may include:
- Topical antifungal creams or ointments, which are applied directly to the affected area
- Oral antifungal medications, which are taken by mouth and work systemically to target the infection
- Medicated cleansers or shampoos, which can help prevent the spread of the infection to other areas of the body
It's essential to follow your doctor's instructions and complete the full course of treatment, even if your symptoms improve before the medication is finished. This will help ensure that the infection is fully treated and reduce the risk of recurrence.
Preventing Yeast Infections of the Skin
There are several steps you can take to reduce your risk of developing a yeast infection on the skin:
- Keep the skin clean and dry, especially in areas prone to moisture, such as the armpits, groin, and under the breasts
- Avoid tight, restrictive clothing that can cause friction and irritation
- Change out of wet clothing, such as swimsuits or workout gear, as soon as possible
- Use a gentle, fragrance-free soap and avoid harsh chemicals or irritants
- Take steps to manage blood sugar levels if you have diabetes or other similar conditions
By practicing good hygiene and being aware of the factors that can contribute to yeast infections, you can help maintain the delicate balance of yeast and bacteria on your skin and prevent infections from occurring.
When to Seek Medical Attention
If you suspect you have a yeast infection of the skin, it's essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment. Don't attempt to self-diagnose or treat your symptoms, as this can lead to complications or worsen your condition. Remember, early intervention is key to effectively treating yeast infections of the skin and preventing potential complications.
Conclusion
Yeast infections of the skin can be uncomfortable and frustrating, but understanding the science behind these infections can help you take steps to prevent them and seek appropriate treatment when necessary. By maintaining proper skin hygiene and being aware of the factors that can contribute to yeast overgrowth, you can help ensure your skin stays healthy and balanced.






Comments
Gary Marks
13 May 2023What a parade of misinformation we’ve been fed about skin yeast, and honestly it makes my blood boil. First, the notion that a simple dab of cream will magically erase the fungal army is a fantasy sold by big pharma to keep us buying tube after tube. The reality is that yeast likes damp, warm pockets like a secret party in your armpits or groin, and it will exploit any broken barrier with a ferocious drive that borders on evil. You think you can just wash it away? No, the fungus builds a bio‑film, a shield that renders ordinary soap useless and forces you into a cycle of itching that feels like tiny knives on your skin. It’s not just about “keeping clean”; it’s about managing moisture, avoiding tight synthetics, and recognizing that antibiotics can open the floodgates for the yeast to swarm like invaders. When your immune system is compromised, whether by stress, steroids, or uncontrolled diabetes, the fungus throws a victory parade and multiplies unchecked. The clinical studies cited in the article barely scratch the surface, ignoring the socioeconomic factors that push people into environments where humidity and lack of proper clothing are the norm. Moreover, the prescription of oral antifungals without considering liver function is a reckless gamble that could end in more harm than good. If you’re still relying on over‑the‑counter ointments, you’re simply feeding the beast with a false sense of security while the underlying imbalance festers. The only way to truly defeat this hidden menace is to combine rigorous hygiene with a balanced microbiome, perhaps even probiotic topicals, and to demand that doctors explain the why behind each treatment. Don’t be a passive victim; demand a comprehensive plan that tackles moisture control, diet, and medication adherence, or you’ll find yourself stuck in an endless loop of rash and irritation that drains both confidence and cash.
Steven Young
13 May 2023It's obvious that the pharma agenda is behind the push for creams and pills they want you to buy every month the fungus just thrives in the gaps they ignore. There's a hidden link between the prescription rates and the lobbyists feeding the industry legitimacy it needs the data they present is cherry‑picked to keep the market alive there is no real push for lifestyle changes beyond a brief mention.
cariletta jones
13 May 2023Great reminder to keep those skin folds dry and breathable; a quick tip is to swap polyester workout gear for cotton after a session to cut down moisture buildup.
Holly Green
14 May 2023Following a doctor’s full course, even when symptoms fade, is the responsible way to avoid the infection coming back and spreading.
Craig E
14 May 2023When we consider the skin as a living ecosystem, respecting the prescribed regimen is akin to honoring a social contract with our own body; neglecting it disrupts the delicate balance and invites chaos.
Marrisa Moccasin
14 May 2023Did you ever notice how the pharmaceutical companies, with their glossy brochures!!!, seem to downplay the role of diet and humidity in favor of endless prescriptions??? It feels like they’re hiding a truth about natural remedies that could free us from this cycle!!!
Caleb Clark
14 May 2023Listen up folks!! If you’re dealing with that itchy, burning feeling, the first step is to get your laundry routine on point!! Wash everything in hot water, use a gentle, fragrance‑free detergent, and dry thoroughly!! Then, swap out any tight underwear for breathable fabrics!! Keep a spare pair of cotton socks handy for workouts!! And don’t forget to apply the antifungal cream exactly as directed – twice a day for the full two weeks, even if you feel better!! Consistency is key, and trust me, your skin will thank you later!!
Ritik Chaurasia
14 May 2023In many cultures we’ve known for centuries that keeping the body dry with natural fibers and regular oiling prevents fungal overgrowth, yet modern medicine keeps ignoring this wisdom while pushing synthetic solutions.
Vandermolen Willis
14 May 2023Stay dry and you’ll win! 😊
Mary Keenan
14 May 2023That’s the simplest truth you can give – no fluff, just keep moisture at bay and you’ve covered half the battle.