Senior Medication Safety: Protecting Elderly Health from Dangerous Drug Interactions
When it comes to senior medication safety, the practice of choosing and managing drugs for older adults to avoid harm while treating illness. Also known as geriatric prescribing, it’s not just about giving the right pill — it’s about avoiding the ones that could hurt more than help. As people age, their bodies process drugs differently. Kidneys slow down. Liver function declines. Muscle mass drops. All of this means a drug that was safe at 50 can become dangerous at 75. The problem isn’t just the number of pills — it’s which ones are in the bottle.
One of the biggest tools doctors use to protect seniors is the Beers Criteria, a regularly updated list of medications that pose higher risks for older adults. Also known as inappropriate drugs for elderly, this guide flags everything from certain antihistamines that cause confusion to sleep aids that increase fall risk. These aren’t just warnings — they’re life-saving alerts. For example, diphenhydramine (found in Benadryl and many sleep aids) is on the list because it blocks acetylcholine, a brain chemical seniors already have less of. The result? Memory lapses, dizziness, even delirium. And it’s everywhere — in cold medicines, allergy pills, and nighttime pain relievers. Many seniors don’t realize they’re taking it because it’s hidden under brand names.
Another hidden danger is medication interactions, when two or more drugs combine to create unexpected, harmful side effects. Also known as drug-drug interactions, these aren’t rare — they’re routine in older patients taking five or more prescriptions. Think of a senior on blood pressure meds who takes a decongestant for a cold. That decongestant can spike blood pressure, undoing months of control. Or someone on warfarin eating inconsistent amounts of vitamin K-rich greens — a small change that throws their INR levels off, risking stroke or bleeding. These aren’t accidents. They’re predictable outcomes of poor coordination between providers, pharmacies, and patients.
What makes this even harder is that many seniors aren’t told why a drug was prescribed — or when to stop it. Doctors focus on treating one condition, but rarely step back to look at the whole picture. A painkiller for arthritis, a statin for cholesterol, an antidepressant for low mood, a diuretic for swelling — each makes sense alone. Together? They can overload the body. The solution isn’t just more pills. It’s fewer, smarter ones. And that starts with asking: Is this still necessary? Is there a safer alternative? Have we checked for interactions?
Below, you’ll find real, practical guides that cut through the noise. From the exact drugs to avoid in older adults to how to safely switch from generics back to brand-name meds, these posts give you the facts — no fluff, no jargon. You’ll learn how to read labels, spot hidden risks, and talk to your doctor with confidence. This isn’t theoretical. These are the tools that keep seniors out of the ER and living well at home.
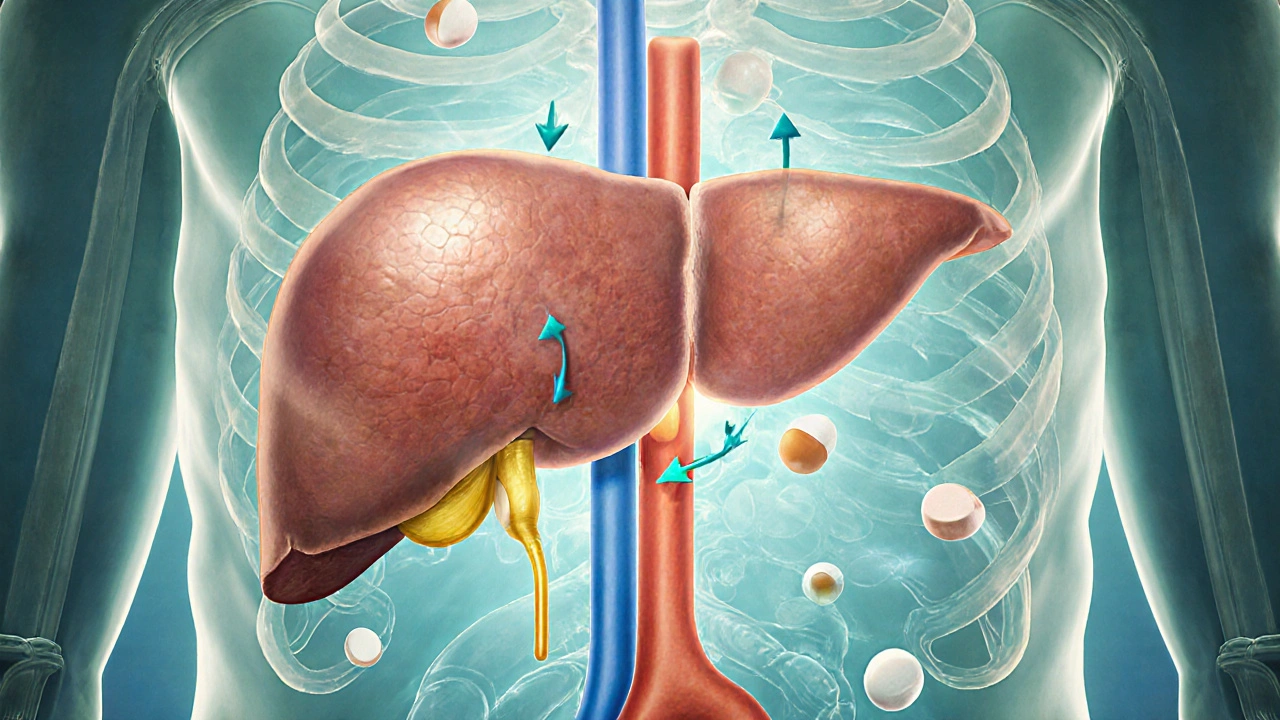
How Liver and Kidney Changes in Older Adults Affect Drug Metabolism
Age-related changes in liver and kidney function alter how drugs are processed in older adults, increasing the risk of adverse reactions. Learn how these changes impact medication safety and what you can do to prevent harm.
Read More




