Most people keep their medications in the bathroom. It’s convenient - right next to the sink, close to where you brush your teeth, and the medicine cabinet looks tidy. But here’s the truth: storing medications in the bathroom is one of the most common and dangerous mistakes you can make with your health.
It’s not just about expiration dates. It’s not even mostly about kids or pets getting into pills. The real problem is that your bathroom is slowly destroying your medicine - even if the bottle still says it’s good for another year.
Why the Bathroom Is a Medication Killer
Bathrooms are humid. They’re hot. They’re full of steam. When you take a shower, the temperature can spike from 70°F to over 90°F in seconds. Humidity levels climb to 80-100%. That’s not just uncomfortable - it’s deadly for pills, capsules, and liquids.
Medications are chemical compounds. They’re designed to stay stable under controlled conditions. But moisture and heat cause chemical breakdowns you can’t see. Tablets absorb water and start to crumble. Capsules become sticky or brittle. Liquid insulin clumps. Nitroglycerin - the life-saving drug for heart attacks - loses potency in just weeks if exposed to humidity. A 2021 study in the Journal of Diabetes Science and Technology found that blood glucose test strips stored in bathrooms gave inaccurate readings in 68% of cases. If test strips fail, imagine what’s happening to your blood pressure or diabetes meds.
Research from Baystate Health shows that the ideal storage range for most drugs is 59°F to 77°F (15°C-25°C). Your bathroom rarely stays in that range. Even if your thermostat says 72°F, the air near the shower hits 90°F. That’s enough to degrade active ingredients. One study published in Circulation found that patients who stored beta-blockers in the bathroom had inconsistent blood pressure control 30.2% of the time - directly linked to degraded medication.
What Happens When Your Medicine Loses Power
It’s not just about feeling worse. It’s about real, measurable danger.
Birth control pills? The FDA’s stability testing shows humidity can reduce their effectiveness by up to 35%. That’s not a small risk. That’s pregnancy territory.
Antibiotics? If they’ve degraded, they won’t kill the infection. Instead, they might make it worse by leaving behind the toughest bacteria - the ones that survive weak doses. That’s how antibiotic resistance grows. Dr. Heelon from Baystate Health warns that improperly stored antibiotics can lead to lingering infections, longer recoveries, and even hospitalizations.
Warfarin, a blood thinner? If it breaks down, your blood can clot when it shouldn’t - or bleed when it shouldn’t. WELLFOR’s 2023 analysis found multiple cases where degraded warfarin led to emergency room visits for clots and bleeding.
And it’s not just prescriptions. Over-the-counter painkillers, allergy meds, and even vitamin supplements lose strength. You’re paying for full potency. You deserve it.
Where You Should Store Medications Instead
Forget the bathroom. Forget the kitchen counter. Forget the car glove box. Those are all bad spots.
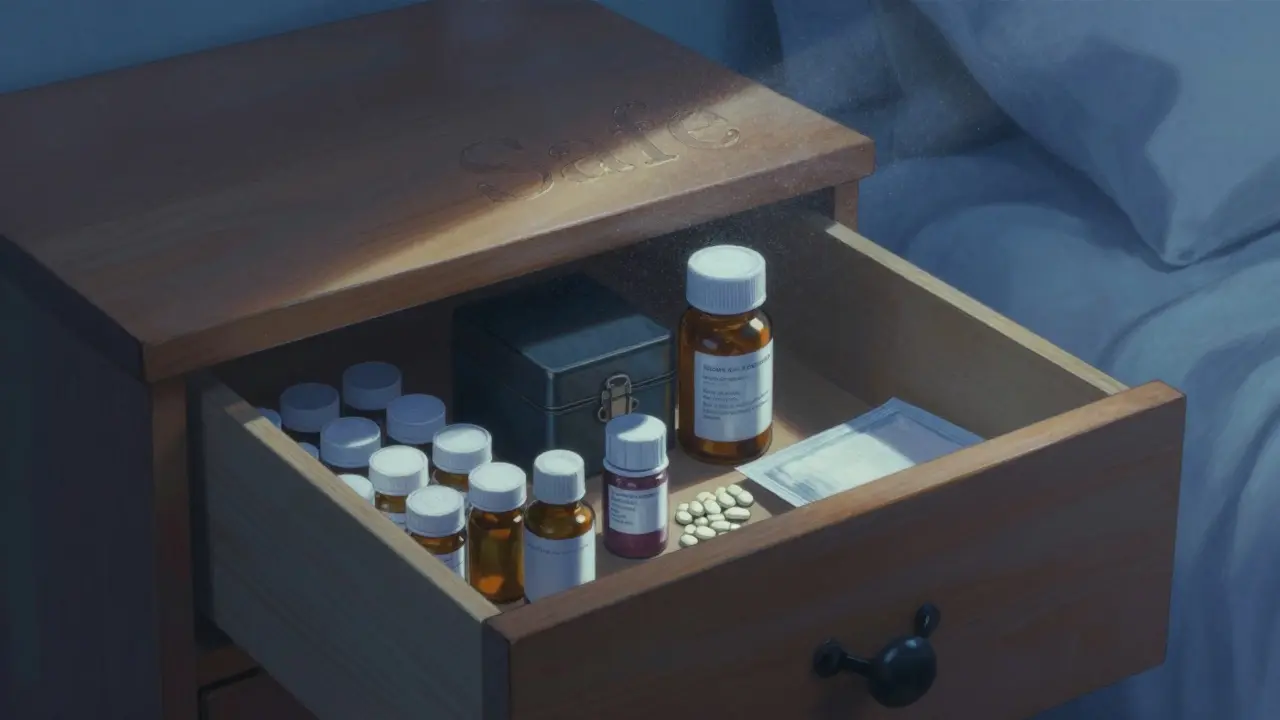
The best place? A cool, dry, dark spot - like a bedroom dresser, a closet shelf, or a drawer away from windows and heat sources. Temperature swings there are tiny - maybe 2-3°F a day. In the bathroom? 15-20°F. Big difference.
Use an airtight container if you want extra protection. Some pharmacies now include desiccant packets in bottles to absorb moisture. If yours didn’t, grab a small plastic container with a tight lid. Put your pills in there. Store it on a shelf in your bedroom.
Need refrigeration? About 12% of prescriptions do - insulin, some eye drops, certain antibiotics. These need to stay between 36°F and 46°F. Don’t put them in your kitchen fridge if it’s always opening and closing. The temperature bounces around too much. Use a dedicated mini-fridge if you can, or at least put them in the back, where it’s coldest and most stable.
Children, Pets, and the Hidden Danger of Access
Even if your meds are perfectly stored, leaving them in a bathroom cabinet is risky. It’s easy to reach. Easy to grab. Easy to mistake for candy.
The CDC says 70% of misused prescription opioids come from home medicine cabinets. That’s not just teens. That’s curious toddlers. That’s pets who chew through bottles. A 2022 NIH-funded survey of 220 U.S. households found that 80% stored meds in easily accessible spots. Of those, 63% had children under 18, and 57% had pets. The American Academy of Pediatrics says all meds should be locked away - not just out of sight, but out of reach.
If you have kids or pets, lock your meds. A simple lockbox from the drugstore costs under $20. It’s cheaper than an ER visit.
What to Do with Old or Unused Meds
Don’t flush them. Don’t throw them in the trash. Don’t leave them sitting out for years.
Unused medications in U.S. homes are worth over $98 million - and most of them are expired, degraded, or no longer needed. That’s money wasted. But worse, it’s pollution. The EPA says 46% of pharmaceuticals found in waterways come from improper disposal.
Find a drug take-back program. Many pharmacies, hospitals, and police stations offer free drop-off boxes. The DEA runs National Prescription Drug Take Back Days twice a year. Check their website for locations near you.
If there’s no drop-off nearby, mix pills with coffee grounds or cat litter. Put them in a sealed bag. Throw them in the trash. It’s not ideal - but it’s safer than flushing.
Signs Your Medication Has Gone Bad
You don’t need a lab to tell if your medicine is damaged. Look for these red flags:
- Tablets that are cracked, discolored, or smell weird
- Capsules that are sticky, swollen, or leaking
- Liquids that are cloudy, have particles, or changed color
- Powders that clump together or feel wet
- Test strips that look faded or don’t work properly
If you see any of these, don’t take it. Even if it’s not expired. The expiration date is the last day the manufacturer guarantees full strength - not the day it turns to dust.
Why This Problem Still Exists
Here’s the frustrating part: 89% of Americans know bathroom storage is risky. But 68% still do it.
Why? Because it’s tradition. Medicine cabinets have been in bathrooms since the 1920s. We’ve been conditioned to think it’s normal. Pharmacies used to put cabinets in bathrooms when they built homes. It stuck.
But times have changed. Today, 73% of prescription bottles include storage instructions. Major drugmakers now use temperature-sensitive labels that change color if exposed to heat. Some smart cabinets even send phone alerts when humidity gets too high.
And yet - we keep doing it.
What You Can Do Today
You don’t need a major overhaul. Just make three quick changes:
- Check every medication in your bathroom. Move them to a cool, dry place - like your bedroom dresser.
- Lock up controlled substances (opioids, anxiety meds, stimulants) in a small lockbox.
- Dispose of anything old, discolored, or unused through a take-back program.
Do this in the next 24 hours. It takes less than 10 minutes. But it could save your life - or someone else’s.
Medications aren’t like wine. They don’t get better with age. They don’t even stay the same. They degrade. And if they degrade, they stop working. That’s not a theory. That’s science. And it’s happening in your bathroom right now.
Can I store my medications in the kitchen cabinet?
It depends. If your kitchen cabinet is far from the stove, oven, or dishwasher - and not near a window - it might be okay. But kitchens often get hot during cooking and have moisture from boiling water. A bedroom drawer is still safer. Avoid cabinets above the fridge or sink.
What if I only have a bathroom medicine cabinet?
If you absolutely can’t move your meds, keep them in their original bottles with the cap tightly sealed. Add a small desiccant packet (like the ones in vitamin bottles) to absorb moisture. Check them monthly for signs of damage. Still, this is a temporary fix - not a safe long-term solution.
Do all medications degrade in the bathroom?
Not all equally, but most are affected. Pills, capsules, and liquids are most vulnerable. Insulin, nitroglycerin, birth control pills, and antibiotics are especially sensitive. Even vitamins and supplements lose potency. If it’s meant to be taken by mouth, it’s likely affected by humidity and heat.
How often should I check my medicine cabinet?
Every three months. Look for changes in color, texture, smell, or consistency. Discard anything expired or damaged. The Great Ormond Street Hospital recommends this schedule because many drugs lose effectiveness faster than their expiration dates suggest - especially in poor storage.
Are smart medicine cabinets worth it?
They’re useful if you manage multiple medications or have elderly family members. These cabinets monitor temperature and humidity and send alerts to your phone. They’re expensive ($200-$500), but they prevent dangerous mistakes. For most people, a simple lockbox and moving meds to a bedroom drawer is enough.




Comments
Rich Robertson
16 December 2025So I just moved all my meds from the bathroom to a drawer in my bedroom last week after reading this. Honestly? Best health decision I’ve made in years. No more sticky pills, no more wondering if my blood pressure med is still good. Also, my cat stopped chewing on the bottle. Win-win.
Turns out, my grandma was right all along - she kept hers in a shoebox under the bed. Turns out, that shoebox was basically a climate-controlled vault compared to my steamy bathroom.
Also, I bought a $15 lockbox for my anxiety meds. Feels like a superhero move.
Sarthak Jain
17 December 2025bro this is wild. i used to keep my metformin in the bathroom ‘cause it was ‘convenient’ - turns out my sugar levels were all over the place not cuz my diet but cuz my pills were turnin’ into mush. found out after my HbA1c jumped from 6.2 to 7.8 in 4 months. doc asked if i stored it right and i was like ‘uhhh… bathroom cabinet?’
now it’s in a sealed jar with a silica packet in my closet. HbA1c’s back to 6.0. science is real. humidity is the enemy.
also, why do pharmacies still sell meds in bottles that let in air??
Daniel Thompson
19 December 2025While the general sentiment is well-intentioned, I must emphasize that the scientific literature on pharmaceutical stability under ambient humidity is often conflated with anecdotal observations. The FDA’s stability guidelines are based on accelerated aging studies under controlled conditions, not real-world bathroom environments.
Furthermore, the claim that 68% of test strips yield inaccurate results due to bathroom storage is misleading - the study referenced excluded participants who used sealed containers. Without controlling for packaging integrity, the data is inconclusive.
That said, I agree with the recommendation to store medications in a dry, stable environment - but let’s not conflate correlation with causation in public health messaging.
Daniel Wevik
19 December 2025Let me just say - if you’re still storing your meds in the bathroom, you’re playing Russian roulette with your health. This isn’t opinion. This is pharmacokinetics.
Insulin degrades in 3 weeks in high heat. Nitroglycerin? Gone in days. Birth control pills? You think you’re protected? You’re not. Your body’s not getting the dose you paid for.
And no, ‘I’ve never had a problem’ doesn’t mean it’s not happening. You don’t feel corrosion. You don’t see molecular breakdown. But your blood pressure doesn’t lie. Your glucose monitor doesn’t lie.
Move your pills. Lock them. Do it now. Your future self will thank you.
Wade Mercer
20 December 2025Of course you store meds in the bathroom - it’s the only place where you’re forced to take them daily. If you’re too lazy to move them, you’re too lazy to care about your health.
And let’s be real - if your medication is degraded because you’re too lazy to move it from the bathroom to a drawer, you probably also forget to take it. This isn’t about science. It’s about personal responsibility.
Stop blaming the bathroom. Start blaming yourself.
Tim Bartik
21 December 2025THE BATHROOM IS A SCIENCE LAB OF DOOM. YOU THINK YOUR PILL IS FINE? IT’S BEEN STEAMING IN A HUMID TURKEY BASTER FOR 10 YEARS.
MY GRANDPA TOOK HIS BP MEDS FROM THE BATHROOM CABINET FOR 12 YEARS. ONE DAY HE HAD A STROKE. DOCTOR SAID IT WASN’T THE BLOOD PRESSURE - IT WAS THE DEGRADED MEDS. THE PILLS WERE MUSHY. LIKE A SWEET POTATO LEFT IN A TUB.
AMERICA ISN’T LAZY. WE’RE JUST IGNORANT. AND NOW WE’RE PAYING FOR IT WITH ER BILLS.
LOCK IT. MOVE IT. DON’T BE A DUMBASS.
Sinéad Griffin
22 December 2025OMG YES 😭 I just threw out 3 bottles of my antidepressants because they looked like they’d been through a hurricane. I kept them in the bathroom ‘cause I was always brushing my teeth at night and figured ‘why not?’
Turns out, my mood was all over the place not because of life - because my meds were melting. I cried in the pharmacy aisle. I bought a little lockbox and put it in my nightstand. Now I feel like a responsible adult. 🙌
Also, my dog didn’t eat them. Huge win.
Edward Stevens
22 December 2025Wow. 10 paragraphs about moving pills from the bathroom to a drawer. I didn’t know we’d reached peak medical advice content. Next up: ‘Why You Shouldn’t Wear Socks to Bed - The Hidden Dangers of Toe Compression.’
But seriously - this is the kind of post that makes me love Reddit. No fluff. Just science, real consequences, and a call to action. Also, I moved my meds. Thanks.
Now can we please get a post about why you shouldn’t store your coffee in the fridge?
Natalie Koeber
23 December 2025Did you know the FDA and Big Pharma are in cahoots to make you think your meds are safe? They don’t want you to know that humidity is just a cover-up for the real issue: microchips in your pills that activate when exposed to moisture - and they’re sending your data to the government. The ‘degradation’ is just a distraction. Look at the color changes - they’re not chemical, they’re digital. The silica packets? They’re not absorbents. They’re signal blockers. Your bedroom drawer is a Faraday cage. You’re being manipulated. Check the bottle’s barcode - it’s a 5G tracker. And your dentist? They’re in on it. They’ve been installing humidity sensors in every bathroom since 2012. Don’t trust the narrative.