When you’re 70, your body doesn’t process medications the same way it did at 30. That’s not just a myth-it’s science. As we age, our liver and kidneys change in ways that directly impact how drugs are absorbed, broken down, and cleared from the body. These changes aren’t subtle. They can turn a safe dose into a dangerous one, and that’s why so many older adults end up in the hospital because of their own medications.
What Happens to the Liver as We Age?
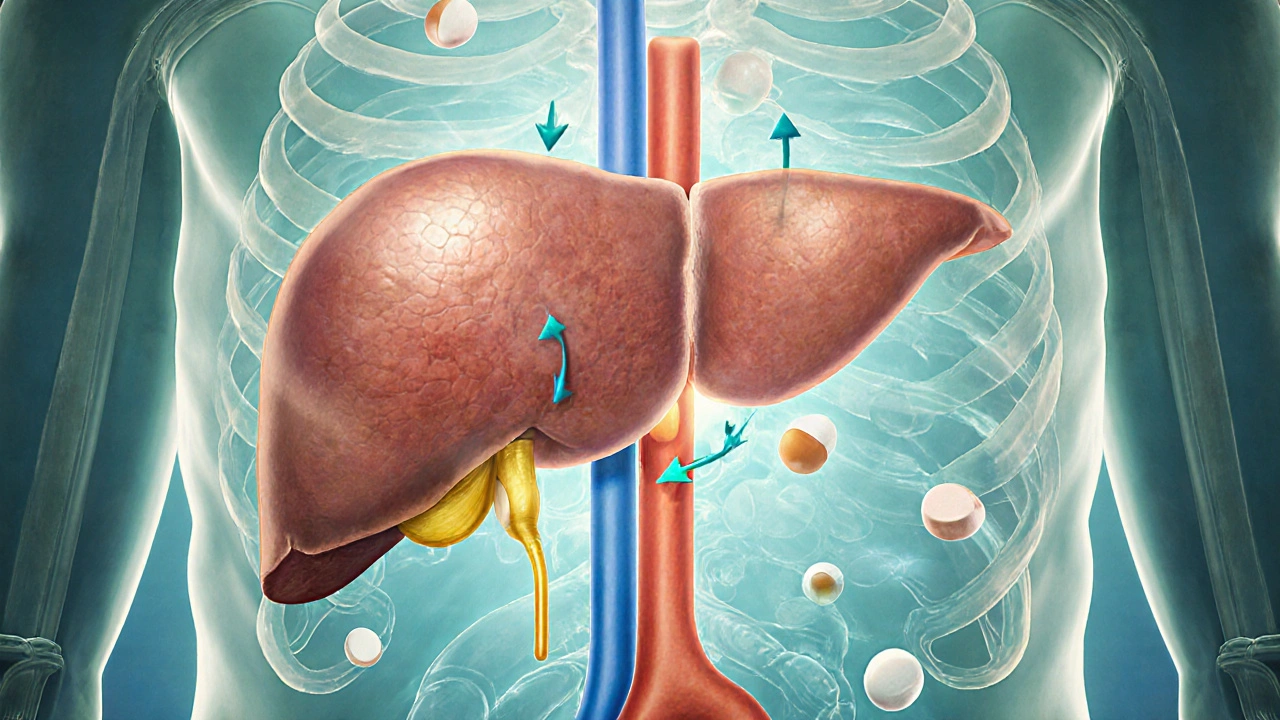
Your liver does the heavy lifting when it comes to breaking down drugs. But after 65, it starts to shrink-by about 30%. Blood flow to the liver also drops by nearly 40%. That means drugs move through it slower. For some medications, that’s not a big deal. For others, it’s life-threatening.
Drugs like propranolol, lidocaine, and morphine are called flow-limited. Their clearance depends almost entirely on how much blood reaches the liver. With less blood flow, these drugs stay in your system longer. A standard dose meant for a 40-year-old can build up to toxic levels in an 80-year-old. One study found that the bioavailability of propranolol can increase by up to 50% in older adults. That’s why some seniors on this heart medication end up with dangerously low blood pressure or a slow heart rate.
On the other hand, drugs like diazepam, phenytoin, and theophylline are capacity-limited. Their metabolism depends more on enzyme activity than blood flow. Here’s the good news: many of these enzymes stay fairly stable with age. So these drugs don’t accumulate as quickly. But don’t assume safety-other factors like kidney function and drug interactions still matter.
There’s another twist: some drugs need to be activated by the liver before they work. These are called prodrugs. Perindopril, an ACE inhibitor used for high blood pressure, is one. If your liver can’t convert it properly, the drug won’t work as intended. That’s why some older patients with high blood pressure seem unresponsive to treatment-they’re not noncompliant. Their liver just can’t do its job anymore.
How Kidney Changes Impact Medication Clearance
Your kidneys filter waste-and a lot of drugs-from your blood. By age 80, most people lose 30% to 50% of their kidney function. That’s measured by glomerular filtration rate, or GFR. But here’s the trap: doctors often rely on serum creatinine to judge kidney health. That’s misleading. As we age, we lose muscle mass. Less muscle means less creatinine is made. So even if your kidneys are failing, your creatinine level might look normal. That’s how people end up on full doses of kidney-cleared drugs like metformin or vancomycin when they shouldn’t be.
Drugs that leave the body mostly through the kidneys need dose adjustments. That includes antibiotics, painkillers like acetaminophen (in high doses), and diabetes meds. The Cockcroft-Gault equation is still widely used to estimate kidney function, but newer formulas like CKD-EPI are more accurate because they don’t factor in race. Many hospitals are switching to CKD-EPI for this reason.
And here’s something many don’t realize: when your kidneys slow down, your liver can slow down too. Studies show that kidney impairment reduces the activity of liver enzymes like CYP3A4. That means even drugs cleared by the liver might build up if your kidneys aren’t working well. It’s a double hit.
Why Older Adults Are at Higher Risk for Bad Reactions
It’s not just about one organ failing. It’s about the perfect storm.
Over 40% of adults over 65 take five or more prescription drugs. That’s called polypharmacy. And with every extra pill, the chance of a bad interaction goes up. A 2019 JAMA study found that people on five or more medications have an 88% higher risk of hospitalization due to drug reactions.
One Reddit user, "CaregiverInMA," shared how their 82-year-old mother started on a standard dose of amitriptyline for nerve pain. Within days, she was dizzy, confused, and falling. Her doctor didn’t realize that amitriptyline is heavily metabolized by the liver-and in older adults, even a small dose can cause severe sedation and delirium. Her dose was cut in half, and her symptoms disappeared.
The FDA estimates that about 10% of hospital admissions in older adults are caused by adverse drug reactions. That’s not just bad luck. It’s preventable. Many of these cases involve drugs that were never tested properly in older populations. Only 38% of participants in new drug trials are over 65. So we’re prescribing based on data from people half their age.
What Doctors Should Do (and Often Don’t)
There are tools to help. The Beers Criteria, updated in 2019, lists drugs that should be avoided or used with extreme caution in older adults. It’s not a suggestion-it’s a guideline backed by decades of evidence. For drugs processed by the liver, it recommends starting at 20% to 40% lower doses for people over 65, and even lower for those over 75.
The STOPP/START criteria help doctors decide what to stop and what to start. A 2020 meta-analysis showed that using these tools reduced adverse drug events by 22%. That’s not a small win-it’s life-changing.
Yet many doctors still rely on age alone. "She’s 80, so give her half the dose" isn’t enough. You need to know: What’s her kidney function? Her liver enzymes? What other drugs is she taking? Is she on an OTC painkiller like acetaminophen? That’s the hidden danger. Acetaminophen causes half of all acute liver failures in older adults-not because it’s toxic, but because the liver can’t process it properly.
What You Can Do as a Patient or Caregiver
You don’t need to be a doctor to protect yourself or a loved one. Here’s what actually works:
- Keep a full list of every medication-prescription, OTC, supplements, and herbal products. Bring it to every appointment.
- Ask: "Is this drug still necessary?" Many seniors stay on meds long after the original reason is gone.
- Ask for a kidney and liver function test before starting a new drug. Don’t assume your doctor already checked.
- Ask if the drug is on the Beers Criteria list. If it is, ask for an alternative.
- Watch for signs of trouble: confusion, dizziness, falls, extreme fatigue, or nausea. These aren’t "just getting old." They could be drug side effects.
One 78-year-old man on vancomycin for a stubborn infection was at risk of kidney damage. His doctor used therapeutic drug monitoring-checking blood levels regularly-and adjusted his dose based on his estimated GFR. He recovered without harm. That’s precision medicine. And it’s possible for anyone.
The Future Is Personalized
There’s new hope. In 2023, the FDA approved the first software tool designed specifically for older adults: GeroDose v2.1. It simulates how a drug will behave in your body based on your age, weight, kidney function, liver enzymes, and other medications. It’s not perfect yet-but it’s a start.
Researchers are also looking at epigenetics. Turns out, your genes don’t just change with age-they get switched on or off by lifestyle, stress, and environment. A 2023 study found 17 methylation sites linked to liver enzyme activity that shift as we get older. That could one day lead to blood tests that tell your doctor exactly how your body will handle a drug-not just guess based on your birthday.
By 2030, experts predict that personalized dosing could cut adverse drug reactions in older adults by 35% to 50%. But that only happens if we stop treating age as a number and start treating it as a biological condition-with real, measurable changes in how the body works.
Why do older adults react differently to medications than younger people?
Older adults have reduced liver mass and blood flow, which slows how drugs are broken down. Kidney function also declines, meaning drugs cleared by the kidneys stay in the body longer. These changes can cause medications to build up to unsafe levels, even at standard doses. It’s not about being "sensitive"-it’s about physiology.
What are the most dangerous drugs for seniors?
According to the Beers Criteria, drugs like benzodiazepines (e.g., diazepam), anticholinergics (e.g., diphenhydramine), and certain antidepressants (e.g., amitriptyline) are high-risk. They can cause confusion, falls, and delirium. Even common OTC meds like acetaminophen can cause liver damage if taken daily over time. Always check if a drug is on the Beers list before starting it.
Can I just reduce my dose by half if I’m over 65?
Not always. Some drugs need only a small reduction; others require a 70% cut. It depends on how the drug is processed. Flow-limited drugs like morphine need bigger reductions than capacity-limited ones like diazepam. Always consult a pharmacist or geriatric specialist before changing any dose.
Why does my doctor keep prescribing the same dose even though I’m older?
Many doctors aren’t trained in geriatric pharmacology. Drug labels often don’t include age-specific dosing, and clinical trials rarely include older adults. That means doctors are guessing. Ask if your medication is on the Beers Criteria list or if your kidney and liver function have been checked recently.
How can I tell if a medication is causing problems?
Look for sudden changes: new dizziness, confusion, memory lapses, loss of appetite, falls, or extreme fatigue. These aren’t normal aging. They’re red flags. If symptoms started after a new medication was added, that’s likely the cause. Don’t wait-talk to your doctor or pharmacist right away.






Comments
Barry Sanders
15 November 2025This is why I stopped trusting doctors after my dad died from a "standard dose" of amitriptyline. They treat 80-year-olds like 40-year-olds with wrinkles. Toxic levels build up silently. No one checks. No one cares. Just another statistic.
Chris Ashley
16 November 2025bro i had my grandma on vancomycin and the doc just gave her the regular dose. she was in and out of the hospital for 3 months. finally found a geriatric pharmacist who said "your kidneys are basically a sieve now." they don’t train docs for this stuff. it’s wild.
kshitij pandey
18 November 2025Thank you for sharing this. My uncle in India is 76 and on 6 medications. I didn’t know about Beers Criteria until now. I showed his doctor the list and he changed 3 drugs. He’s sleeping better, no more falls. Small changes save lives. We just need to speak up.
Brittany C
19 November 2025The Cockcroft-Gault vs. CKD-EPI discrepancy is a systemic failure. Even in academic hospitals, legacy formulas persist due to EMR inertia. CYP3A4 suppression secondary to renal impairment is underrecognized in clinical practice-this paper from JAMA Internal Medicine last year details the bidirectional organ crosstalk.
Sean Evans
20 November 2025OMG I KNEW IT. 😤 My aunt got prescribed diazepam for "anxiety" at 79. She was hallucinating, peeing on the floor, and calling me at 3am thinking I was her dead husband. The doctor said "it’s just aging." NO. IT’S MEDICAL NEGLIGENCE. 💀 This is why I won’t let my parents near a pharmacy without me.
Anjan Patel
21 November 2025Let me tell you something - this entire system is rigged. Big Pharma doesn’t test on old people because they don’t want to see the side effects. Doctors don’t care because they’re paid to prescribe, not to think. And patients? They’re too scared to ask. It’s a death sentence wrapped in a prescription bottle. 🚨
Scarlett Walker
23 November 2025My mom started taking melatonin for sleep at 72. Turns out it’s metabolized by the liver and she was getting dizzy. We cut it out and switched to magnesium glycinate - no more falls, no more confusion. Sometimes the fix is simple. Just listen to your body.
Hrudananda Rath
24 November 2025It is with profound regret that I observe the lamentable state of contemporary pharmacological practice, wherein the physiological decrepitude of geriatric patients is not merely overlooked, but actively disregarded in favor of archaic, pediatric-derived dosing paradigms. This is not medicine - it is negligence masquerading as protocol.
Brian Bell
26 November 2025So many people think "I’m old, I just need to slow down" - but dizziness isn’t aging, it’s a warning. My dad’s doctor didn’t even check his creatinine until he fell and broke his hip. Now he’s on a new med regimen. He’s walking again. Don’t wait for the fall. Ask for the test.
Nathan Hsu
26 November 2025Acetaminophen? Daily? Over 65? That’s like playing Russian roulette with your liver. I’ve seen it. I’ve lost friends. The FDA says 4,000 mg/day is safe - but for older adults? That’s a death sentence. Cut it in half. Or better yet - skip it. Turmeric works better anyway.
Ashley Durance
28 November 2025Let’s be real - the Beers Criteria is outdated. It ignores polypharmacy synergies and doesn’t account for frailty indices. And the GeroDose software? Still uses crude linear models. Until we incorporate epigenetic methylation markers and dynamic clearance algorithms, we’re just rearranging deck chairs on the Titanic.
Scott Saleska
28 November 2025I’m a nurse. I’ve seen this a hundred times. Someone comes in confused after a new script. We check meds. Oh - they’ve been on the same dose of sertraline since they were 60. Now they’re 82. We halve it. They’re lucid in 48 hours. It’s not magic. It’s math. And no one does the math.