Precautions: Stay Safe with Medications and Online Pharmacies
Small precautions can prevent big problems. Before starting any medicine, check allergies, current prescriptions, and health conditions. If anything feels off, stop and talk to a professional. This page gives practical tips to help you spot risks, avoid scams, and keep your treatments on track.
Before you start any medication
Read the label and the patient leaflet every time, even for drugs you’ve used before. Watch allergy warnings, dosing instructions, and storage notes. Ask your doctor or pharmacist about interactions with other prescriptions, over-the-counter drugs, or supplements. For example, some antibiotics and antifungals lower birth-control effectiveness, and acne drugs like isotretinoin require strict pregnancy precautions.
Keep a simple medication list on your phone with names, doses, and times. Share it with every provider you see. If a drug needs lab checks — like liver or blood monitoring — schedule them and follow up on results. Stop the medicine and get help if you see sudden rash, trouble breathing, yellow skin, severe belly pain, or extreme fatigue.
Shopping online and practical safety checks
Pick online pharmacies with a real address, clear contact info, and a license or seal from a recognized regulator. Avoid sites that sell controlled drugs without a prescription or offer unusually low prices. If a site refuses to share a pharmacist phone number or asks for weird payment methods, walk away.
Keep order receipts and tracking numbers. Inspect packages when they arrive: seals should be intact and pills should match photos or descriptions. If anything looks wrong — different color, smell, or packaging — don’t take it. Contact the seller for a return and report the problem to your local regulator.
Certain people need extra care: pregnant or breastfeeding people, seniors on many meds, kids (who need weight-based doses), and those with liver or kidney disease. For benzodiazepines, opioids, and some psychiatric drugs, get a clear taper plan from your prescriber to avoid withdrawal.
Finish an antibiotic course unless your doctor says otherwise — stopping early can promote resistance. For pain meds, use the lowest effective dose for the shortest time and secure leftovers to prevent misuse. Use pill boxes or phone alarms for chronic meds, and don't drive or operate heavy machinery if a medicine affects your alertness.
Dispose of unused meds safely — many pharmacies offer take-back programs. Don’t flush most medicines down the toilet. Keep medicines locked away from children and visitors who might misuse them. Note any unusual reactions with dates and photos; clear notes help your provider act fast.
Use trusted interaction checkers (pharmacy apps or sites like Drugs.com) before combining prescriptions and supplements. Watch common culprits: grapefruit with some heart meds, St. John's wort with antidepressants and birth control, and NSAIDs with blood thinners. For severe allergic reactions, loss of consciousness, or heavy bleeding, call emergency services or poison control immediately.
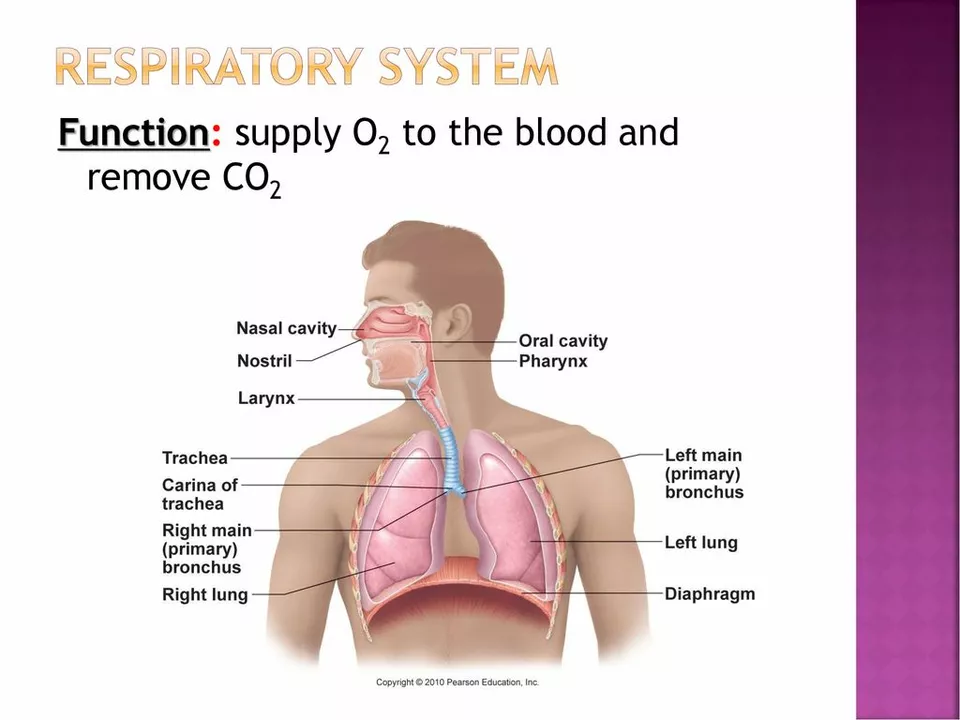
Acetaminophen and your respiratory system: What you need to know
As a blogger, I recently came across some important information about acetaminophen and its effects on our respiratory system. I discovered that acetaminophen, a common pain reliever, can potentially cause respiratory problems when taken in excess or in combination with other medications. It's crucial for us to be aware of these potential risks and pay attention to the recommended dosages. I also learned that those with pre-existing respiratory conditions should be extra cautious when using acetaminophen. Stay tuned for a more detailed post on this topic to help you better understand the connection between acetaminophen and your respiratory system.
Read More




