Diabetes: Practical Tips to Manage Blood Sugar, Meds, and Daily Risks
Diabetes doesn’t have to control your life. Small, consistent steps make the biggest difference: regular blood sugar checks, steady routines for meds, smart food choices, and knowing when to act. Read on for clear, useful tips you can use today.
Start with monitoring. If you use a glucose meter or continuous monitor, check patterns, not single numbers. Track fasting, before-meal, and bedtime readings for a week. Are mornings high? That could mean the dawn phenomenon or late-night snacks. Are post-meal spikes common? Try smaller portions of starchy foods and add protein or fiber to your plate.
Daily habits that actually work
Keep it simple: choose three habits and stick with them for 4 weeks. Examples that pay off fast:
- Take meds at the same time every day — set an alarm or use a pillbox.
- Move for 10–20 minutes after meals; even a short walk blunts blood sugar spikes.
- Use the plate method: half non-starchy veggies, one quarter lean protein, one quarter carbs.
If you’re on insulin, learn the timing and action of each dose. Fast-acting insulin covers meals; long-acting covers baseline needs. Talk to your prescriber before changing doses. If you use oral meds like metformin, know common side effects (stomach upset early on) and when to report symptoms.
Low blood sugar happens — be ready. The 15-15 rule works: eat 15 grams of fast-acting carbs (glucose tabs, 4 oz juice, or 3–4 glucose gels), wait 15 minutes, then recheck. If still low, repeat. Keep a source of carbs with you and tell close contacts how to help.
Practical checks and safety tips
Feet, eyes, kidneys, and heart are the places diabetes hits over time. Quick ways to protect them:
- Foot check daily: any cuts, blisters, or numbness? See care right away.
- Annual eye exam by an optometrist/ophthalmologist.
- Get blood pressure and cholesterol checked; meds like ACE inhibitors or statins often help protect your heart and kidneys.
Watch drug interactions. If you take other prescriptions for heartburn, infection, or pain, some combinations can alter blood sugar or increase side effects. Use a reliable drug-info tool or our medication guides to check interactions before adding anything new.
Practical meal ideas: swap white rice for cauliflower rice or 1/3 cup cooked quinoa; swap sugary drinks for sparkling water with lemon; add a boiled egg or a handful of nuts to meals to slow carb absorption. These changes cut spikes without feeling like punishment.
Finally, plan for sick days. Illness often raises blood sugar. Check more often, stay hydrated, and follow your sick-day plan from your care team — and call them if sugars stay unusually high or you can’t eat for more than 24 hours.
Want more detail on medications, interactions, or how certain drugs affect diabetes? Check our guides and medication reviews on RxStore-365 for up-to-date, practical information that helps you make safer choices every day.
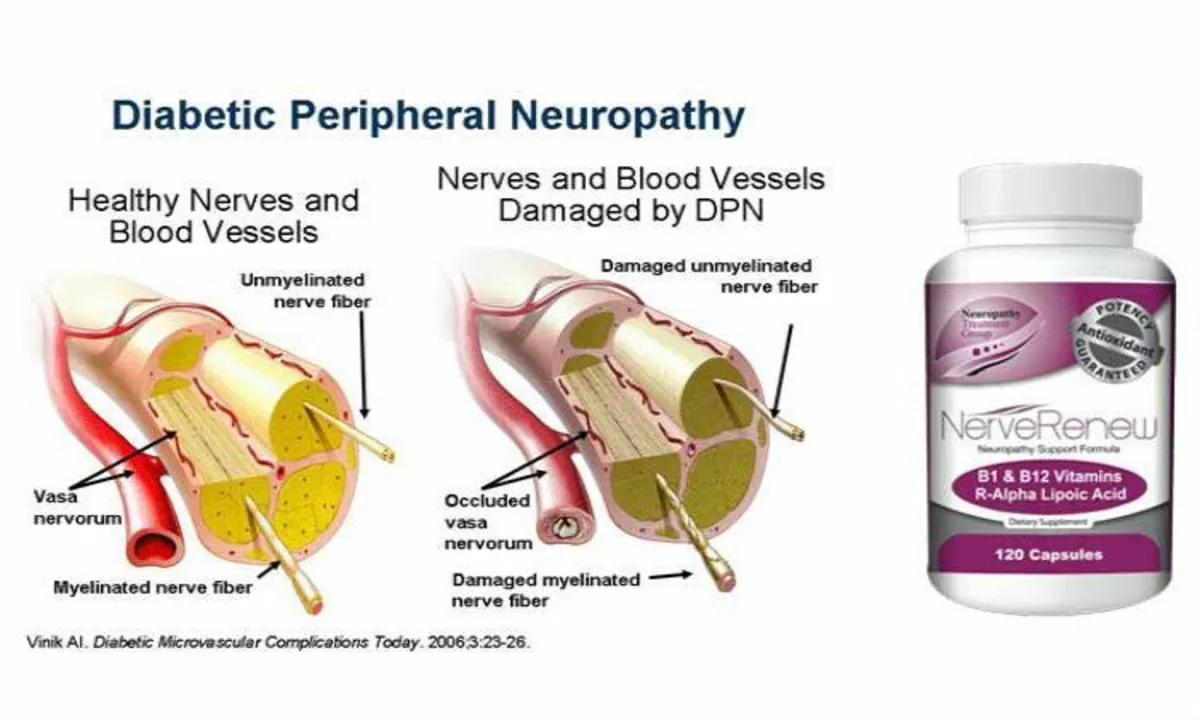
Diabetic Peripheral Neuropathy and Vision Loss: What You Need to Know
As a diabetic, I've been learning about the risks of diabetic peripheral neuropathy and vision loss. In just five sentences, here's what you need to know: Diabetic peripheral neuropathy is a common complication of diabetes, affecting the nerves in our legs and feet, leading to pain and numbness. This condition can also cause vision loss if it affects the nerves in our eyes. It's essential to manage our blood sugar levels and have regular check-ups with our healthcare providers to prevent these complications. Early detection and treatment can help reduce the risk of severe consequences. Remember, staying informed and proactive about our health is the key to living a better life with diabetes.
Read More