Key Takeaways
- Primaquine is the only drug that targets dormant liver stages of malaria.
- Alternatives like Mefloquine or Chloroquine work on blood stages but not hypnozoites.
- G6PD deficiency is the main safety hurdle for Primaquine; other agents have different contraindications.
- Cost and dosing convenience vary widely - single‑dose regimens (e.g., Artemisinin) are cheap but may need combination therapy.
- Choosing the right drug depends on species (Plasmodium vivax vs Plasmodium falciparum), patient risk factors, and regional resistance patterns.
What Is Primaquine?
Primaquine is a 8‑aminoquinoline antimalarial approved by the World Health Organization (WHO) for radical cure of Plasmodium vivax and Plasmodium ovale infections. It uniquely eliminates hypnozoites - the dormant liver forms that cause relapses.
The drug is administered orally, usually as a 14‑day course (0.5 mg/kg per day) for radical cure, or as a single 0.25 mg/kg dose for transmission blocking in endemic areas.
How Does Primaquine Work?
Primaquine interferes with the parasite’s mitochondrial electron transport chain, generating oxidative stress that kills both blood‑stage parasites and liver‑stage hypnozoites. This dual action makes it the only medication that can achieve a true “radical cure”.
Because the mechanism relies on oxidative damage, patients with G6PD deficiency risk hemolysis - a consideration that drives the need for alternative drugs when testing is unavailable.
When Is Primaquine Needed?
Clinical guidelines recommend Primaquine in three main scenarios:
- Radical cure after a confirmed Plasmodium vivax infection to prevent relapse.
- Mass drug administration for malaria elimination programs, using a single low dose to block transmission.
- Relapse prevention in travelers returning from endemic regions where Plasmodium vivax is prevalent.
If a patient cannot take Primaquine (e.g., severe G6PD deficiency), clinicians turn to other agents, each with its own strengths and limits.

Top Alternatives to Primaquine
Below is a snapshot of the most commonly used antimalarial alternatives, focusing on those that can replace Primaquine in specific contexts.
- Mefloquine - effective against blood‑stage Plasmodium falciparum, used for prophylaxis.
- Chloroquine - cheap, good for chloroquine‑sensitive Plasmodium vivax, but resistance limits use.
- Artemisinin and its derivatives (e.g., artemether‑lumefantrine) - fast‑acting blood‑stage killers, often combined with partner drugs.
- Atovaquone‑Proguanil (Malarone) - well‑tolerated, used for prophylaxis and treatment of uncomplicated malaria.
- Doxycycline - cheap, works for prophylaxis, but requires daily dosing and can cause photosensitivity.
Side‑by‑Side Comparison
| Drug | Mechanism | Primary Indication | Typical Dose | Major Side Effects | Contraindications | Cost (US, 2025) |
|---|---|---|---|---|---|---|
| Primaquine | Oxidative damage to mitochondria (8‑aminoquinoline) | Radical cure of P. vivax/P. ovale | 0.5 mg/kg daily ×14 days (or 0.25 mg/kg single dose) | Hemolysis (G6PD), nausea, insomnia | Severe G6PD deficiency, pregnancy (first trimester) | ≈ $2‑$4 per 15‑tablet pack |
| Mefloquine | Inhibits parasite heme polymerization | Prophylaxis & treatment of P. falciparum | 250 mg weekly (prophylaxis) or 1250 mg single dose (treatment) | Neuropsychiatric effects, dizziness | History of psychosis, seizures | ≈ $15‑$20 per 250‑mg tablet |
| Chloroquine | Inhibits heme detoxification | Sensitive P. vivax & P. malariae | 25 mg/kg over 3 days | Retinal toxicity (long term), pruritus | Retinal disease, cardiac block | ≈ $0.10‑$0.20 per tablet |
| Artemisinin‑based combos | Free radical generation causing parasite death | Uncomplicated P. falciparum | Artemether‑lumefantrine 4 tablets twice daily ×3 days | Vomiting, QT prolongation | Severe cardiac disease, pregnancy (first trimester) | ≈ $6‑$9 per treatment course |
| Atovaquone‑Proguanil | Inhibits mitochondrial electron transport (atovaquone) + DHFR inhibition (proguanil) | Prophylaxis & treatment of mixed‑species malaria | 250 mg/100 mg tablet daily | Abdominal pain, rash | Severe renal/hepatic impairment | ≈ $30‑$40 per 4‑tablet pack |
| Doxycycline | Inhibits protein synthesis (30S ribosomal subunit) | Prophylaxis for all malaria species | 100 mg daily | Photosensitivity, esophagitis | Pregnancy (first trimester), children <8 yr | ≈ $0.20‑$0.30 per tablet |
Making the Choice: When to Pick Primaquine vs an Alternative
Think of the decision as a flowchart:
- Is the infection caused by P. vivax or P. ovale? If yes, Primaquine (or tafenoquine) is the only drug that eradicates hypnozoites.
- Does the patient have confirmed normal G6PD activity? If a point‑of‑care test is unavailable, consider a short‑course alternative like Doxycycline for prophylaxis, but note it won’t clear liver stages.
- Is there known chloroquine resistance in the region? If resistance is high, skip chloroquine and move to an ACT (artemisinin‑based combination therapy) for blood‑stage clearance.
- Are there neuropsychiatric concerns? Avoid Mefloquine in patients with anxiety or depression.
- What’s the budget? For low‑resource settings, chloroquine or doxycycline may be cheaper, but efficacy and safety must align with local resistance patterns.
In short, Primaquine shines when you need to prevent relapse. If relapse isn’t a concern-or you can’t test G6PD-pick an alternative that matches the species, resistance profile, and patient tolerability.
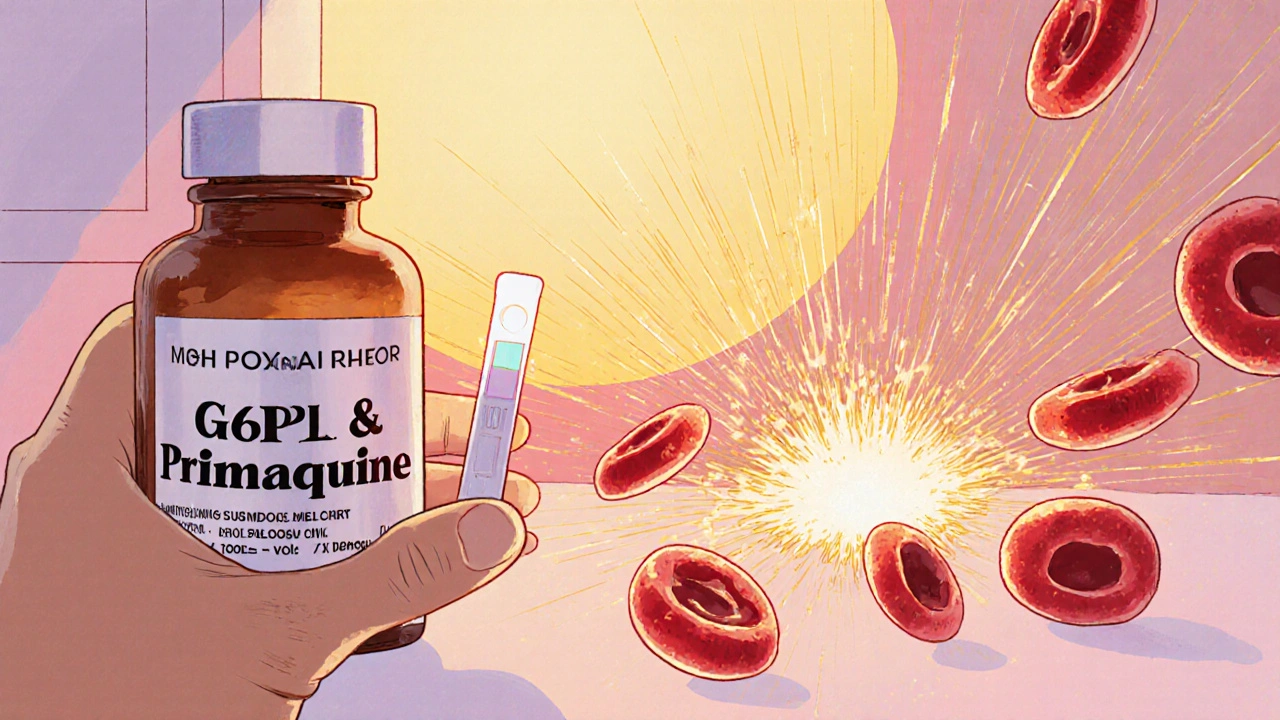
Safety Spotlight: G6PD Deficiency and Hemolysis
G6PD deficiency affects roughly 400 million people worldwide, with higher prevalence in sub‑Saharan Africa, the Mediterranean, and parts of Asia. The enzyme protects red blood cells from oxidative damage; Primaquine’s oxidative mechanism can trigger rapid hemolysis in deficient individuals.
Guidelines recommend:
- Quantitative G6PD testing before a 14‑day Primaquine regimen.
- Using a low‑dose (0.25 mg/kg single) regimen for mass drug administration only when the population’s prevalence of severe deficiency is <5 %.
- Considering tafenoquine (single‑dose) only if quantitative G6PD testing is available, as it shares the same hemolysis risk.
If testing isn’t possible, clinicians often default to Atovaquone‑Proguanil or Doxycycline, accepting that liver stages may persist.
Cost, Availability, and Practical Considerations in 2025
Supply chains have improved since the COVID‑19 pandemic, but regional differences remain. In most high‑income countries, Primaquine is an off‑patent generic, costing under $5 for a full 14‑day pack. In low‑income settings, WHO-prequalified versions are distributed free through malaria elimination campaigns.
Alternatives vary widely:
- Chloroquine is still the cheapest, often <$0.15 per tablet, but resistance limits its use.
- Mefloquine and Artemisinin combos can cost $10‑$20 per treatment, reflecting higher manufacturing costs.
- Atovaquone‑Proguanil remains the most expensive, often covered by insurance for travelers.
When prescribing, factor in not just drug price but also the need for G6PD testing, follow‑up visits, and patient adherence (e.g., a 14‑day Primaquine course versus a weekly Mefloquine dose).
Frequently Asked Questions
Can I take Primaquine if I am pregnant?
Primaquine is generally avoided in the first trimester because safety data are limited. Some guidelines allow use in later pregnancy if the benefit outweighs risk, but G6PD testing is still required.
What is the difference between Primaquine and tafenoquine?
Both are 8‑aminoquinolines targeting hypnozoites. Tafenoquine is a single‑dose option, while Primaquine needs a 14‑day regimen. Tafenoquine shares the same G6PD‑related hemolysis risk but requires a quantitative test before any dose.
Is there a resistance problem with Primaquine?
Resistance to Primaquine is rare, mainly because the drug targets liver stages that are less exposed to drug pressure. However, treatment failures can still occur if patients are G6PD deficient and the drug is stopped early.
How do I know if I need a liver‑stage drug?
If your malaria test identified P. vivax or P. ovale, you need a liver‑stage agent like Primaquine or tafenoquine to prevent relapse.
What side effects should I watch for on Primaquine?
Common issues include nausea, abdominal cramps, and insomnia. The most serious is hemolysis in G6PD‑deficient patients, which can cause dark urine, jaundice, and rapid drop in hemoglobin.
Choosing the right antimalarial hinges on species, patient factors, and local resistance. Primaquine remains unmatched for clearing dormant liver forms, but it demands careful G6PD screening. When that isn’t feasible, alternatives like Mefloquine, Artemisinin-based combos, or Atovaquone‑Proguanil fill the gaps. By matching drug properties to the clinical scenario, you can safely and effectively treat malaria while minimizing relapse risk.







Comments
Dahmir Dennis
24 October 2025Ah, the noble quest for the perfect antimalarial, as if humanity hasn't already squandered centuries on half‑baked solutions. Primaquine, that glorified toxin, proudly claims the exclusive right to eradicate hypnozoites, yet it conveniently forgets that most of the world can't even afford a basic G6PD test. One might argue that prescribing a drug with a known risk of hemolysis without guaranteed screening is an act of moral bankruptcy. But fear not, the pharmaceutical industry swoops in with flashy marketing, promising “radical cure” while ignoring the bitter reality of resource‑poor settings. Meanwhile, alternatives like mefloquine and chloroquine parade their cheapness, pretending virtue by staying out of the liver stage altogether. The irony is palpable: we celebrate a drug that kills parasites in two stages while simultaneously condemning patients to potential severe anemia. And yet, WHO guidelines persist, as if the bureaucratic stamp of approval absolves us of ethical responsibility. The cost‑effectiveness argument is also a stale relic, because when a patient suffers a life‑threatening hemolytic crisis, no amount of dollars saved on a tablet can repair the damage. Moreover, the supposed convenience of a 14‑day regimen is a cruel joke for those who cannot adhere to daily dosing in remote villages. The single‑dose transmission‑blocking strategy sounds like a superhero move, yet it leaves the individual patient exposed to the same G6PD pitfalls. One cannot help but marvel at the sheer hubris of proclaiming Primaquine as the indispensable hero while skulking behind the veil of “if you can test, use it”. In the grand theater of global health, we should be staging plays that prioritize safety over glorified pharmacology. Let us, for once, champion drugs that are both effective and universally accessible without a labyrinth of diagnostics. Until we can guarantee G6PD testing for every malaria‑endemic region, the claim of Primaquine’s supremacy remains a moral illusion. The alternatives, flawed as they may be, at least respect the limits of what can be safely administered. So, before we continue to idolize a molecule that demands such stringent oversight, perhaps we should redirect our enthusiasm toward truly equitable solutions.
Kester Strahan
28 October 2025From a pharmacokinetic standpoint, the hepatic bioavailability of primaquine is heavily influenced by CYP2D6 polymorphisms, which you might have missed in the standard WHO chart. Moreover, the oxidative stress pathway mediated by NADPH oxidase is not just a side-effect but a key driver of hemolytic events in G6PD-deficient popuplations. The cost-benefit analysis, if we look at the incremental cost‑effectiveness ratio (ICER), actually favours atovaquone‑proguanil in areas where point‑of‑care G6PD testing is absent. Yet the guidelines still push primaquine as the gold standard, definatly an oversight in realis world implementation. You could also consider the parasite's schizont‑stage susceptibility, which is often under‑reported in clinical trial endpoints. So, integrating genotype‑guided dosing could mitigate the risk, but that requires infrastructure that many endemic regions lack.
HILDA GONZALEZ SARAVIA
31 October 2025Primaquine’s unique ability to target dormant hypnozoites makes it indispensable for P. vivax eradication, but the drug’s safety profile mandates a careful assessment of G6PD status. In practice, a simple qualitative point‑of‑care test can identify most severe deficiencies, allowing clinicians to adjust the dose or choose an alternative. For travelers, a single low‑dose regimen (0.25 mg/kg) can block transmission without significant hemolysis risk, especially when combined with a blood‑stage therapy. When it comes to cost, generic primaquine remains one of the cheapest options, typically under $5 for a full course, which is a major advantage in low‑resource settings. However, adherence to the 14‑day regimen is a challenge; patient education and reminder tools are essential to achieve a true radical cure.
Amanda Vallery
4 November 2025If you cant get a G6PD test, use mefloquine; it’s safer for those patients.
Marilyn Pientka
7 November 2025Let us dispense with the naïve optimism that permeates most lay discussions of antimalarial therapy and confront the stark reality: Primaquine is a pharmacological relic, revered only by those too enamored with its 'unique' liver‑stage activity to acknowledge its glaring drawbacks. The hyper‑technical jargon surrounding oxidative mechanisms and mitochondrial disruption is nothing more than an intellectual smokescreen, designed to distract from the fact that a drug causing hemolysis in a substantial portion of the global population cannot be touted as a universal solution. In regions where G6PD deficiency prevalence exceeds 5 %, the indiscriminate deployment of primaquine amounts to reckless negligence, masquerading as preventive medicine. Alternatives such as atovaquone‑proguanil or the artemisinin‑based combination therapies, while not perfect, exhibit safety profiles that align with the ethical imperatives of modern clinical practice. One must also critique the WHO’s dogmatic adherence to primaquine, a stance that betrays a bureaucratic inertia rather than evidence‑based adaptability. The intellectual elite must therefore champion a paradigm shift, prioritizing patient safety over antiquated notions of 'radical cure'.
Jordan Levine
10 November 2025🔥💥 Absolutely! The drama of a drug that can both save lives and wreak havoc is unstoppable! 💊⚡️ We need bold moves, not half‑hearted guidelines! 🇺🇸🚀
Carla Taylor
14 November 2025Great overview! Love how you broke down each option – makes choosing treatment feel less scary.
Michelle Capes
17 November 2025Totally agree 😊 The info is super helpful, especially the table – makes stuff crystal clear :)
Dawn Bengel
21 November 2025Only the cheap drugs matter.
junior garcia
24 November 2025The fight against malaria needs heroes, and every pill is a soldier marching toward victory.
Dason Avery
28 November 2025Indeed, each treatment path mirrors our own choices in life – we seek balance between risk and hope, weaving a tapestry of courage and care. 🌟
Casey Morris
1 December 2025While the data presented is comprehensive, one must, however, consider the broader epidemiological context, the socioeconomic factors, and the practical feasibility of implementing such regimens in remote settings; otherwise, the conclusions may be, in effect, overly optimistic.
Teya Arisa
5 December 2025Ms. Morris, your observation is duly noted; the integration of epidemiological nuance with therapeutic strategy is indeed paramount. 😊
Doreen Collins
8 December 2025Remember, you’re not alone in navigating these choices – reach out to your network, share experiences, and stay informed.