Arthritis & Depression Risk Assessment
This tool helps estimate your risk of developing depression based on arthritis-related symptoms and lifestyle factors. Please answer the following questions honestly.
Your Risk Assessment
Living with joint pain is rough, but it’s the emotional fallout that often sneaks up unnoticed. When arthritis flares up, many people find their mood sinking, energy draining, and motivation wavering. This isn’t a coincidence-there’s a solid arthritis depression link that clinicians and patients are learning to spot early. Below we break down why the two conditions mingle, how the body’s chemistry fuels the cycle, and what practical steps can break it.
Understanding Arthritis
Arthritis is a group of joint disorders characterized by inflammation, stiffness, and pain. The most common forms are osteoarthritis, driven by wear‑and‑tear, and rheumatoid arthritis, an autoimmune attack that targets synovial tissue. In 2024, more than 58 million adults in the U.S. reported a doctor‑diagnosed arthritis condition, and prevalence climbs sharply after age 45.
Key symptoms include swelling, reduced range of motion, and chronic discomfort that can last for years. Because joints are essential for daily tasks-from gripping a coffee cup to climbing stairs-persistent pain quickly erodes independence.
Why Depression Often Follows Joint Disease
Depression is a mood disorder marked by persistent sadness, loss of interest, and impaired functioning. Studies from the Arthritis National Research Institute in 2023 show that people with rheumatoid arthritis are up to twice as likely to meet clinical criteria for major depressive disorder compared to the general population.
The relationship isn’t one‑way. While chronic pain can wear down emotional resilience, depressive symptoms-like low motivation and poor sleep-can amplify the perception of pain, creating a feedback loop that’s hard to break.
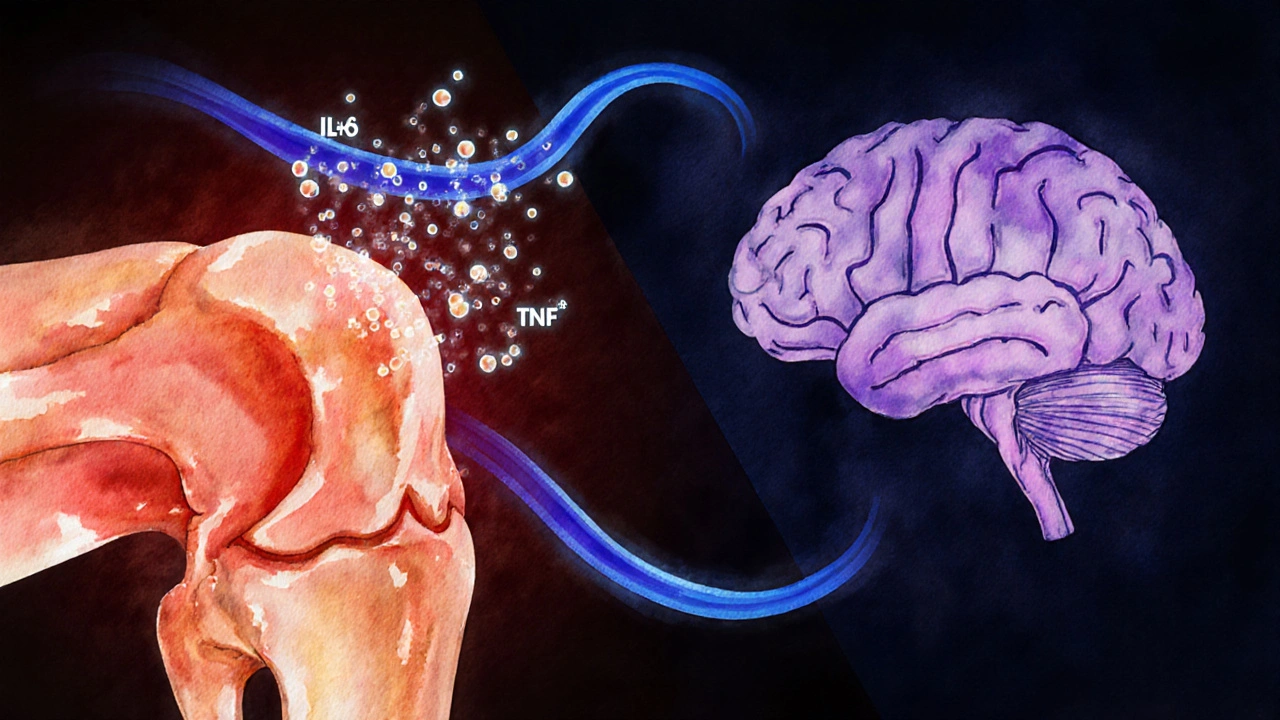
Biological Pathways That Connect Inflammation and Mood
Inflammation sits at the heart of both conditions. When joints inflame, immune cells release cytokines such as interleukin‑6 (IL‑6) and tumor necrosis factor‑alpha (TNF‑α). These messengers don’t stay confined to the joint; they travel through the bloodstream and cross the blood‑brain barrier, where they can disturb neurotransmitter balance.
Two neurotransmitters are especially vulnerable:
- Serotonin (a mood‑stabilizing chemical) often drops when inflammatory cytokines surge, leading to irritability and low mood.
- Cortisol (the stress hormone) spikes in response to chronic pain, and prolonged elevation can blunt the brain’s reward pathways.
Neuroimaging studies in 2022 revealed that patients with high C‑reactive protein-a marker of systemic inflammation-show reduced activity in the prefrontal cortex, a region critical for emotional regulation.
Lifestyle Factors that Worsen Both Conditions
Beyond biology, everyday habits can tip the scales:
- Physical inactivity leads to muscle weakening, joint stiffness, and higher pain scores. Sedentary time also correlates with higher rates of depressive symptoms.
- Sleep disruption caused by night‑time joint pain reduces restorative REM cycles, a known risk factor for mood disorders.
- Social isolation-whether from staying home due to limited mobility or feeling misunderstood-feeds a sense of hopelessness that fuels depression.
These factors interact, making the twin burden feel inevitable unless interventions target both the body and the mind.
Managing the Dual Challenge: Integrated Treatment Strategies
Effective care hinges on a blend of medical, psychological, and lifestyle approaches. Below is a side‑by‑side view of common therapies for arthritis and depression, highlighting where they overlap.
| Approach | Primary Goal (Arthritis) | Primary Goal (Depression) | Effect on the Other Condition | Typical Use |
|---|---|---|---|---|
| Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs) | Reduce joint inflammation and pain | - | Pain relief can improve mood; however, side‑effects may worsen anxiety | Short‑term flare management |
| Selective Serotonin Reuptake Inhibitors (SSRIs) | - | Elevate serotonin to alleviate depressive symptoms | Some SSRIs have modest anti‑inflammatory properties | Moderate to severe depression |
| Physical Therapy & Exercise | Restore joint range, strengthen muscles | Boost endorphins, reduce stress | Improved mobility cuts down pain‑related mood drops | Ongoing maintenance |
| Cognitive Behavioral Therapy (CBT) | - | Restructure negative thought patterns | Teaches coping skills for pain flare‑ups | Chronic depression, pain‑related anxiety |
| Social Support Programs | Encourage activity, reduce isolation | Provide emotional validation, reduce loneliness | Both conditions benefit from increased engagement | Community groups, peer counseling |
Notice how many therapies hit both targets. A combined plan-say, a low‑dose NSAID for flare control plus weekly CBT-often yields faster mood improvements than tackling either issue alone.

When to Seek Professional Help
If you notice any of these signs, it’s time to talk to a clinician:
- Persistent sadness or loss of interest lasting more than two weeks.
- Significant weight change, sleep disturbances, or thoughts of self‑harm.
- Pain that interferes with daily tasks despite medication.
- Feeling hopeless about managing your arthritis.
Rheumatologists can adjust disease‑modifying drugs, while mental‑health providers can assess for major depressive disorder and prescribe appropriate therapy. Integrated clinics-where both specialties collaborate-are becoming more common in major Canadian hospitals, offering a one‑stop approach.
Practical Tips for Daily Living
Even without a formal program, small shifts can lighten the load:
- Morning stretch routine: 5‑minute gentle range‑of‑motion moves (ankle circles, shoulder rolls) reduce stiffness before the day’s activities.
- Mindful breathing: 4‑7‑8 technique (inhale 4 seconds, hold 7, exhale 8) lowers cortisol spikes during pain flare‑ups.
- Schedule “joy breaks”: set a 15‑minute slot for a hobby-reading, music, or a short walk-so mood‑boosting dopamine gets a regular hit.
- Track symptoms: Use a simple app or notebook to log pain level, sleep quality, and mood rating; patterns often reveal triggers you can avoid.
- Lean on community: Join a local arthritis support group (Toronto Arthritis Society hosts weekly meetings) or an online forum where shared experiences cut feelings of isolation.
These habits reinforce each other. Better sleep improves pain tolerance; moving a little each day keeps joints lubricated and releases endorphins that lift mood.
Frequently Asked Questions
Can arthritis medication cause depression?
Some drugs, especially high‑dose corticosteroids, can affect mood and trigger irritability or depressive symptoms. Discuss any mood changes with your rheumatologist; they may adjust dosage or switch to a medication with a lower psychiatric side‑effect profile.
Is it normal to feel anxious about flare‑ups?
Yes. Anticipating pain activates the brain’s threat circuitry, which can heighten anxiety. Techniques like progressive muscle relaxation and CBT help reframe these worries into actionable coping steps.
Do anti‑inflammatory diets help mood?
Eating foods rich in omega‑3 fatty acids, antioxidants, and fiber-such as salmon, berries, and leafy greens-reduces systemic inflammation. Lower inflammation often translates to modest improvements in depressive symptoms, especially when combined with regular exercise.
How quickly can therapy impact my pain levels?
Psychological interventions like CBT typically show measurable reductions in pain perception within 6‑8 weeks. The goal isn’t to eliminate pain but to reshape how the brain interprets those signals, lowering the emotional distress attached to them.
Should I avoid all NSAIDs if I’m depressed?
Not necessarily. Short‑term NSAID use can be crucial for flare control, which may indirectly improve mood by reducing pain. However, long‑term high‑dose use can increase cardiovascular risk and sometimes worsen anxiety; always discuss duration and dosage with your doctor.






Comments
Karen Nirupa
8 October 2025Dear community, recognizing the interplay between chronic joint pain and mood disturbances is essential for holistic care.
When arthritis limits daily activities, feelings of frustration and sadness can naturally arise, and acknowledging this connection fosters compassion.
Quinn Comprosky
12 October 2025Arthritis pain can be relentless and it often feels like a weight that never lifts.
Each flare up can drain your energy and push you toward a low mood.
When sleep is disrupted by joint stiffness you miss restorative rest.
Day after day the constant discomfort wears down optimism.
Social activities become harder to attend when movement is painful.
This isolation can deepen feelings of hopelessness.
Research shows that inflammatory processes in the body may affect brain chemistry.
Thus the physical and emotional strands are tightly woven together.
Managing pain with physiotherapy and medication can lighten the emotional load.
Equally important is building a support network that understands the daily struggle.
Mind‑body techniques such as meditation have been shown to reduce perceived pain and uplift mood.
Keeping a routine of gentle exercise can improve joint function and release endorphins.
Regular check‑ins with a mental health professional can catch depressive symptoms early.
Nutrition rich in omega‑3 fatty acids may also play a role in reducing inflammation and supporting brain health.
Overall a comprehensive approach that addresses both the body and mind offers the best chance for resilience.
Thomas Ruzzano
16 October 2025Honestly if you think a little ache can’t mess with your head you’re living in denial.
The science is crystal clear – chronic inflammation fuels mood swings like a rude alarm clock.
Stop making excuses and get professional help before the darkness takes over.
Ignore the warning signs and you’ll pay the price in endless gloom.
Dan Tenaguillo Gil
19 October 2025Friends, it’s vital to recognize that the link between arthritis and depression isn’t just a coincidence but a bidirectional relationship.
When pain spikes, stress hormones rise, which can alter neurotransmitter balance and pave the way for low mood.
Conversely, depressive states can lower pain tolerance, creating a vicious cycle that traps many patients.
Breaking this loop starts with open communication; sharing your struggles with a trusted clinician can lead to tailored treatment plans.
Physical therapy that emphasizes gentle range‑of‑motion exercises can improve joint health without overwhelming pain.
Complementary strategies such as cognitive‑behavioral therapy have been shown to reframe negative thoughts associated with chronic discomfort.
Additionally, ensuring adequate sleep hygiene – perhaps by using supportive pillows and maintaining a regular bedtime – can dramatically improve both pain perception and emotional stability.
Remember, you’re not alone; community support groups provide a space to exchange coping tactics and emotional encouragement.
Tiffany Owen-Ray
23 October 2025It’s fascinating how our bodies and minds converse in whispers and shouts, and arthritis seems to amplify the whispers until they become a roar of despair.
When you acknowledge that pain isn’t just a physical signal but also an emotional messenger, you open doors to holistic healing.
Consider integrating mindfulness practices that teach you to observe pain without judgment; this can diminish its emotional impact.
Pairing such mental tools with low‑impact activities like swimming or tai chi creates a synergy that nurtures both joints and spirit.
Don’t underestimate the power of a balanced diet rich in antioxidants; foods like berries and leafy greens help quell inflammation that fuels both aches and sadness.
And always keep a journal of your symptoms – patterns often emerge that guide you toward the most effective interventions.
Ultimately, the journey is personal, but you have a toolbox of strategies waiting to be explored.
Jill Brock
27 October 2025Stop playing victim – your misery is a choice.
Ellie Chung
31 October 2025Arthritis is a sneaky beast that loves to steal your sunshine.
Don’t let it hijack your happiness.
Sophia Simone
3 November 2025While many attribute depressive tendencies solely to psychological factors, the immunological cascade triggered by arthritic inflammation warrants equal scrutiny.
Neglecting this physiological pathway risks oversimplifying a complex condition.
Clinical guidelines should therefore integrate anti‑inflammatory strategies alongside traditional psychotherapy.
Only then can we hope to address the root causes rather than merely treating symptoms.
Juan Sarmiento
7 November 2025Hey folks, dealing with joint pain can feel like battling a storm, but you’ve got a crew cheering you on.
Finding the right balance of medication, movement, and mental health support can turn the tide.
Don’t hesitate to reach out to friends or online communities – sharing lifts the weight.
Remember, every small step you take is a victory over both pain and gloom.
Together we can navigate this rough sea and find calmer waters.
Patrick McVicker
11 November 2025Yo, chronic pain can really mess with your vibe 😕.
Make sure to check in with a therapist if you’re feeling down – it’s legit help.
Also, try short walks, they can boost mood and keep joints moving 😊.
Liliana Phera
15 November 2025If you think ignoring the mental toll of arthritis is acceptable, you’re perpetuating a cycle of suffering.
Our brains react to constant nociceptive input, reshaping mood pathways in ways that demand attention.
Wake up to the fact that emotional health is as crucial as joint health, and demand integrated care now.
Dean Briggs
19 November 2025From a philosophical standpoint, the body can be seen as a vessel for experience, and chronic arthritis transforms that vessel into a constant reminder of limitation.
Yet, this very limitation can become a catalyst for personal growth if approached mindfully.
Collaborative treatment plans that involve rheumatologists, psychologists, and physical therapists embody this holistic vision.
By sharing insights across disciplines, patients receive nuanced strategies that address both pain and mood.
For example, incorporating biofeedback can teach patients to modulate stress responses that exacerbate inflammation.
Simultaneously, group therapy offers communal validation, reducing the isolation that fuels depression.
In essence, a unified approach honors the complex interplay of body and mind.
Sadie Speid
22 November 2025Let’s get moving! Even gentle stretching releases endorphins that brighten your mood.
Consistent activity, no matter how light, helps keep inflammation in check.
Pair it with a balanced diet and regular sleep, and you’ll notice a shift in both pain and outlook.
You’ve got the power to boost your own wellbeing.
Sue Ross
26 November 2025I’m curious how many of you have tried journaling your pain levels alongside mood ratings.
Tracking these patterns can reveal triggers you might otherwise miss.
Has anyone noticed a correlation between flare‑ups and specific stressors?
Sharing your observations could help others spot hidden links.
Let’s keep the discussion evidence‑based and supportive.
Rohinii Pradhan
30 November 2025It is disappointing to observe the persistent misunderstanding of the biochemical nexus between rheumatoid pathology and affective disorders.
Many resources trivialize this connection, offering superficial advice that borders on negligent.
A rigorous approach demands that clinicians prescribe anti‑inflammatory agents concurrently with mood‑stabilizing therapy when indicated.
Furthermore, patient education must include clear explanations of cytokine‑mediated neurotransmitter alterations.
Only through such comprehensive instruction can we mitigate the propagation of misinformation.
I urge the community to demand higher standards of scientific accuracy.
Anna-Lisa Hagley
4 December 2025The data suggests a statistically significant correlation between chronic inflammatory markers and depressive symptomatology.
However, causality remains ambiguous without longitudinal studies.
Thus, any therapeutic recommendation should be tempered with caution.
Overstating the link risks inflating patient anxiety.
A Walton Smith
7 December 2025It's another fad.
Theunis Oliphant
11 December 2025Behold the tragedy of a body betraying its own spirit.
The joints ache, the mind weeps.
Only the enlightened understand the depth of this suffering.
Yet society offers cheap pills and empty words.
True cure lies in disciplined mind and body.
India Digerida Para Occidente
15 December 2025Friends, let’s bridge the gap between physical pain and emotional health with compassion and science.
Listening to each other's stories fosters empathy and uncovers hidden patterns.
When we combine medical treatment with honest conversation, we create a powerful antidote to despair.
Assertively seek multidisciplinary care – rheumatology, psychology, nutrition – all play a role.
Your journey need not be solitary; community strength amplifies healing.
Together we can rewrite the narrative of arthritis‑induced depression.