Diabetes Medication Comparison Tool
Select Your Health Profile
Answer these questions to see which diabetes medication class might be most appropriate for you.
Recommended Medication Options
| Medication Class | Key Benefits | Key Considerations |
|---|---|---|
| SGLT2 Inhibitors | 0.5-0.8% A1C reduction 2-3kg weight loss 27% reduced heart failure risk | ⚠️ Risk of genital infections ⚠️ Increased dehydration risk |
| GLP-1 Agonists | 1.0-1.5% A1C reduction 3-5kg weight loss Strong cardiovascular benefits | ⚠️ Requires injections ⚠️ Common side effects (nausea, GI issues) |
| DPP-4 Inhibitors | 0.5-0.7% A1C reduction Minimal weight change Low risk of hypoglycemia | ⚠️ Less effective for weight loss ⚠️ Modest A1C reduction |
Key Takeaways
- Forxiga (dapagliflozin) is an SGLT2 inhibitor that lowers blood sugar, helps with weight loss, and reduces heart‑failure risk.
- Canagliflozin and empagliflozin share the same class but differ in kidney safety profiles and cardiovascular outcomes.
- GLP‑1 agonists such as liraglutide offer stronger A1C drops and weight loss but require injection.
- DPP‑4 inhibitors (sitagliptin) are oral, have modest A1C impact, and cause fewer side effects.
- Choosing the right drug depends on kidney function, heart health, cost, and personal preferences.
What is Forxiga (dapagliflozin)?
When treating type2 diabetes, Forxiga is the brand name for dapagliflozin, an SGLT2 (sodium‑glucose co‑transporter‑2) inhibitor. It works by blocking the kidney’s ability to re‑absorb glucose, letting excess sugar leave the body through urine. FDA approval came in 2014, and the drug is now used in over 30 countries.
Typical dosing starts at 5mg once daily, with a possible increase to 10mg based on blood‑sugar response. Clinical trials show an average A1C reduction of 0.5‑0.8% and a modest weight loss of 2‑3kg. Importantly, Forxiga has demonstrated a 27% reduction in hospitalization for heart failure in patients with established cardiovascular disease.
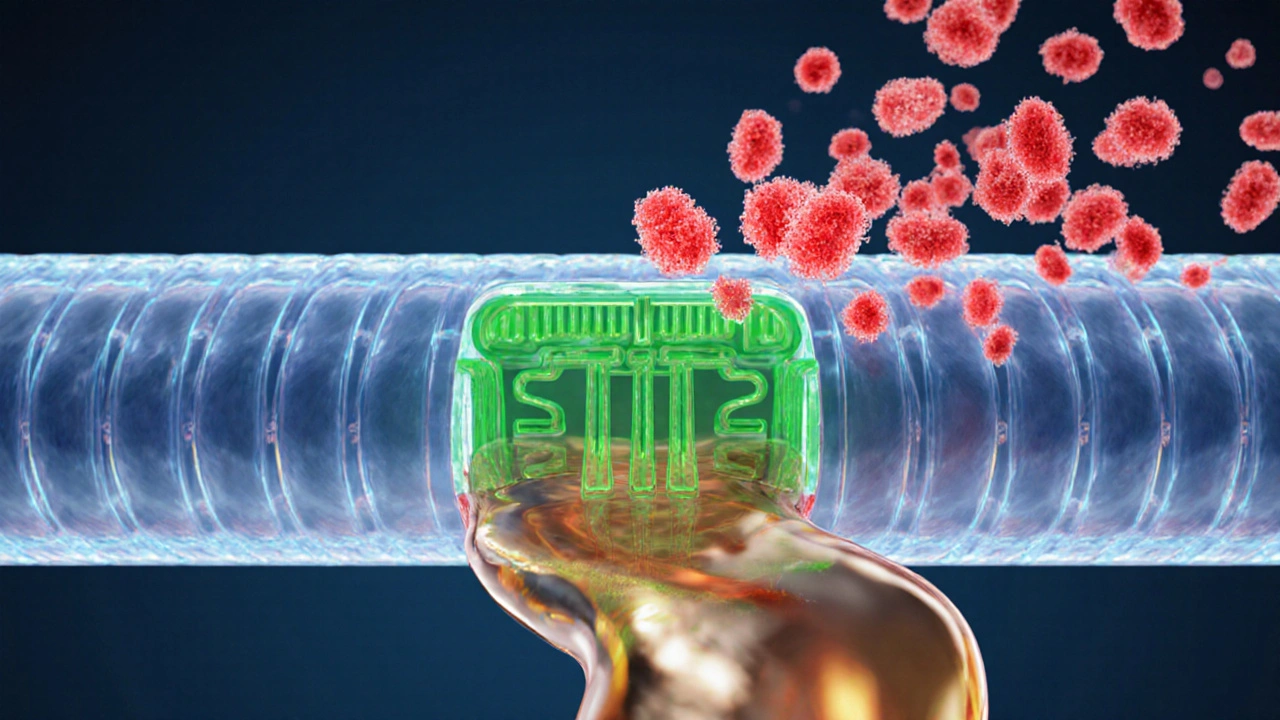
How SGLT2 inhibitors work - the class in a nutshell
All SGLT2 inhibitors share a core mechanism: they inhibit the SGLT2 protein in the proximal tubule of the kidney, which normally re‑absorbs about 90% of filtered glucose. By blocking this protein, the drugs increase urinary glucose excretion (UGE) by roughly 60‑80g per day.
The class benefits include:
- Lowered blood glucose independent of insulin.
- Reduction in systolic blood pressure (3‑5mmHg).
- Weight loss from calorie loss via glucose.
- Cardiovascular and renal protection that go beyond glycemic control.
Common side effects are genital mycotic infections, urinary tract infections, and a slight increase in dehydration risk. Rare but serious risks include ketoacidosis and, for some agents, lower‑leg amputation.
Top alternatives within the SGLT2 class
The two biggest competitors to Forxiga are Canagliflozin (brand name Invokana) and Empagliflozin (brand name Jardiance). Both hit the same target but differ in dosing flexibility and safety nuances.
- Canagliflozin: FDA‑approved in 2013, typical dose 100mg daily, can be increased to 300mg. Shows up to 1.0% A1C reduction. Notable for a higher risk of lower‑leg amputation, leading to a boxed warning in 2017.
- Empagliflozin: Came to market in 2014. Standard dose 10mg daily, titratable to 25mg. The EMPA‑REG OUTCOME trial highlighted a 38% drop in cardiovascular death, making it the go‑to choice for patients with heart disease.
All three agents share the same contraindications - type1 diabetes, severe renal impairment (eGFR<30mL/min/1.73m²), and active ketoacidosis.
Non‑SGLT2 alternatives - other oral and injectable options
When patients can’t tolerate SGLT2 inhibitors or need additional glucose control, clinicians turn to other classes.
- Liraglutide (Victoza) - a GLP‑1 receptor agonist given daily by injection. Offers 1.0‑1.5% A1C reduction, 3‑5kg weight loss, and proven heart‑failure benefit.
- Sitagliptin (Januvia) - a DPP‑4 inhibitor taken once daily. Modest 0.5‑0.7% A1C drop, neutral weight effect, and very low hypoglycemia risk.
- Metformin - the first‑line biguanide. Reduces A1C by 1.0‑1.5% and promotes modest weight loss, but contraindicated in advanced kidney disease (eGFR<30).
Each alternative brings its own pros and cons, which we’ll line up in the comparison table below.
Choosing the right drug - factors to weigh
Deciding whether Forxiga or an alternative fits a patient’s profile involves balancing several variables.
- Kidney function: SGLT2 agents need an eGFR≥45mL/min/1.73m² for full dosing; below that, dose reduction or a switch to metformin or DPP‑4 inhibitors is safer.
- Cardiovascular risk: Empagliflozin and liraglutide carry the strongest heart‑failure data, while canagliflozin adds a modest reduction in major adverse cardiac events (MACE).
- Weight goals: SGLT2 inhibitors and GLP‑1 agonists both promote weight loss; DPP‑4 inhibitors are weight‑neutral.
- Administration preference: Oral pills (Forxiga, canagliflozin, empagliflozin, sitagliptin, metformin) are convenient; however, patients comfortable with injections may achieve better A1C control with liraglutide.
- Cost & insurance: Generic dapagliflozin isn’t widely available yet, so brand‑name pricing matters. Canagliflozin and empagliflozin have multiple generics as of 2025, often lowering out‑of‑pocket costs.
By scoring each factor, patients can create a simple decision matrix: high heart‑failure risk → empagliflozin; concern about amputations → avoid canagliflozin; preference for oral, moderate A1C drop → Forxiga; desire for strongest weight loss → liraglutide (if injection is acceptable).

Cost and insurance snapshot (2025 US market)
Pricing data are averages from pharmacy benefit managers and can vary by plan.
| Drug | Average monthly retail cost (USD) | Typical insurance copay |
|---|---|---|
| Forxiga (dapagliflozin) | $420 | $30‑$45 |
| Canagliflozin (generic) | $300 | $20‑$35 |
| Empagliflozin (generic) | $280 | $15‑$30 |
| Liraglutide (injection) | $950 | $75‑$150 |
| Sitagliptin (generic) | $250 | $15‑$25 |
| Metformin (generic) | $10 | $0‑$5 |
Most commercial plans place SGLT2 inhibitors in Tier3, meaning a higher copay. Patients with Medicare PartD often qualify for a $4‑$10 copay under the $4,000 catastrophic threshold.
Quick comparison table
| Drug | Class | A1C reduction (typical) | Weight effect | Cardio‑renal benefit | Common side effects | FDA approval year |
|---|---|---|---|---|---|---|
| Forxiga | SGLT2 inhibitor | 0.5‑0.8% | ‑2‑‑3kg | ↓ HF hospitalizations (27%) | Genital yeast, UTIs, dehydration | 2014 |
| Canagliflozin | SGLT2 inhibitor | 0.7‑1.0% | ‑2‑‑4kg | ↓ MACE, ↑ amputation risk | UTIs, bone fractures | 2013 |
| Empagliflozin | SGLT2 inhibitor | 0.6‑0.9% | ‑2‑‑3kg | ↓ CV death (38%) | Genital infections, ketoacidosis | 2014 |
| Liraglutide | GLP‑1 agonist | 1.0‑1.5% | ‑3‑‑5kg | ↓ HF, ↓ MACE | Nausea, vomiting, pancreatitis | 2010 |
| Sitagliptin | DPP‑4 inhibitor | 0.5‑0.7% | Neutral | Neutral | Headache, nasopharyngitis | 2006 |
| Metformin | Biguanide | 1.0‑1.5% | ‑2‑‑3kg | Neutral | GI upset, lactic acidosis (rare) | 1995 |
Frequently Asked Questions
Can I take Forxiga if I have chronic kidney disease?
For patients with eGFR≥45mL/min/1.73m², Forxiga can be used at the standard dose. If eGFR falls between 30‑44, a reduced 5mg dose is allowed in some regions, but many clinicians switch to a DPP‑4 inhibitor or insulin when kidney function declines further.
Why do SGLT2 inhibitors cause genital infections?
Because they increase sugar in the urine, creating a fertile environment for yeast and bacteria. Good hygiene and staying well‑hydrated lower the risk. In most cases infections are mild and respond to a short course of antifungal medication.
Is Forxiga better than metformin for weight loss?
Metformin does cause modest weight loss, but Forxiga typically yields a slightly larger reduction (2‑3kg vs. 1‑2kg) and adds a clear heart‑failure benefit. However, metformin remains first‑line because of its long safety record and low cost.
Can I combine Forxiga with a GLP‑1 agonist?
Yes. The combination is often prescribed for patients needing aggressive A1C control and maximal weight loss. Studies show additive A1C drops of up to 1.5% and no major safety signals beyond the individual drug profiles.
What should I do if I experience dizziness on Forxiga?
Dizziness can signal dehydration or low blood pressure, especially after the first weeks. Increase fluid intake, avoid standing up too quickly, and monitor blood pressure. If symptoms persist, talk to your prescriber; dose adjustment may be required.




Comments
Paige Crippen
12 October 2025Have you ever wondered why the big pharma giants push Forxiga so hard? They're probably hiding a massive data set that shows worse side‑effects than they admit, but the FDA gets cozy with the lobbyists and sweeps it under the carpet. The marketing blitz is just a distraction while they collect even more glucose from our urine to line their offshore accounts. Remember, every new “breakthrough” comes with a hidden clause in the fine print that benefits the shareholders, not the patients.
sweta siddu
21 October 2025Wow, that's a wild take! 😅 Even if some of those theories sound extreme, it’s good to stay skeptical and read the full prescribing information. The SGLT2 class does have proven cardiovascular benefits, which can be a lifesaver for many. Just keep an eye on hydration and genital hygiene, and you’ll minimize the common side effects. 🌟 Stay informed and stay healthy!
Ted Mann
30 October 2025In the grand theater of metabolic control, Forxiga is but a fleeting actor on the stage of mortality, trading glucose for the illusion of autonomy. Its modest A1C dip tempts the desperate, yet the underlying metabolic entropy remains untouched, merely masked by diuresis. The drug whispers promises of weight shedding, but the body’s homeostatic rebellion may erupt as ketoacidosis in the shadows. Thus, one must contemplate whether chemical coercion truly tames the diabetic beast or simply shrouds its ferocity in a veil of clinical numbers.
Shaquel Jackson
8 November 2025Honestly, the data looks fine but the side‑effects are a hassle 😐.
Amelia Liani
17 November 2025Indeed, the narrative you paint captures the existential tension that patients often feel when entrusting their glycemic destiny to a pill. However, the empirical evidence demonstrates a statistically significant 0.5‑0.8 % reduction in HbA1c, coupled with a 27 % decrease in heart‑failure hospitalizations-a quantitative testament to its clinical merit. While the philosophical musings are compelling, the measurable outcomes cannot be dismissed outright. Let us therefore balance the metaphysical with the measurable, acknowledging both the hope and the hazards inherent in such therapy.
shikha chandel
26 November 2025They conceal the renal risks, plain and simple.
Zach Westfall
5 December 2025Behold the marvel of SGLT2 inhibition It siphons sugar out of the bloodstream like a silent thief granting patients modest weight loss and a whisper of cardiovascular protection yet the price is whispered in the shadows of genital infections and dehydration
Pranesh Kuppusamy
14 December 2025From a pharmacological perspective the SGLT2 inhibitors such as dapagliflozin present a mechanism of action that bypasses insulin pathways thereby offering benefit to patients with insulin resistance however the data also reveal a spectrum of adverse events ranging from urinary tract infections to rare cases of ketoacidosis the clinical decision must weigh these factors meticulously
Garrett Gonzales
22 December 2025Forxiga (dapagliflozin) belongs to the sodium‑glucose cotransporter‑2 (SGLT2) inhibitor class, which exerts its antihyperglycemic effect by reducing renal glucose reabsorption and promoting glucosuria. Pharmacokinetic studies indicate a peak plasma concentration (Cmax) achieved within 1–2 hours post‑dose, with an elimination half‑life of approximately 12 hours, supporting once‑daily administration. In pivotal phase III trials such as DECLARE‑TIMI 58, dapagliflozin achieved an average HbA1c reduction of 0.5–0.8 % versus placebo, meeting the primary efficacy endpoint. Moreover, the same trial demonstrated a 17 % relative risk reduction in composite cardiovascular outcomes, driven largely by a decrease in hospitalization for heart failure. Renal outcomes were also favorable, with a slowed decline in estimated glomerular filtration rate (eGFR) over a median follow‑up of 4.2 years. The safety profile is characterized by an increased incidence of genital mycotic infections, reported in 5–7 % of patients, which are typically mild and responsive to standard antifungal therapy. Volume depletion events occurred in roughly 3 % of subjects, necessitating caution in individuals on concomitant diuretics. Ketoacidosis, although rare (<0.1 %), remains a serious adverse event, particularly in patients with low carbohydrate intake or acute illness. Dose adjustments are not routinely required for mild to moderate renal impairment (eGFR ≥ 45 mL/min/1.73 m²), but the drug is contraindicated in severe renal dysfunction (eGFR < 30 mL/min/1.73 m²). Drug–drug interaction potential is low, as dapagliflozin is minimally metabolized by CYP enzymes and is primarily excreted unchanged. In the context of combination therapy, it synergizes well with metformin, DPP‑4 inhibitors, and GLP‑1 receptor agonists, allowing for robust glycemic control without heightened hypoglycemia risk. Cost‑effectiveness analyses have shown that the incremental cost per quality‑adjusted life year (QALY) gained is acceptable in healthcare systems with a willingness‑to‑pay threshold of $50,000–$100,000. Real‑world data corroborate the trial findings, indicating sustained HbA1c reductions and cardiovascular benefits across diverse patient populations. Patient adherence is generally high, attributed to the oral route of administration and the modest side‑effect burden. Nevertheless, clinicians should counsel patients on proper genital hygiene and maintain vigilance for signs of dehydration. In summary, dapagliflozin offers a multifaceted therapeutic profile that addresses glycemic, weight, and cardiovascular endpoints, positioning it as a valuable option in the contemporary armamentarium against type 2 diabetes.
Aman Deep
31 December 2025Picture a sunrise over the Himalayas, each ray a molecule of dapagliflozin slipping through the nephron gates like a silent monk meditating on sugar liberation 🌄 the body whispers gratitude as excess glucose drifts away like a kite in the wind the heart, once burdened, now beats a steadier rhythm echoing the ancient drums of vitality however the mind must stay wary of the hidden dragons of infection that dwell in warm, moist corners of our anatomy 🐉 gentle hydration and careful watch become the mantra for travelers on this metabolic pilgrimage
Teknolgy .com
9 January 2026Honestly, it’s just another pill that promises the moon 🌙 and delivers a modest dip in numbers. The hype feels manufactured, and the side‑effects are the real plot twist. If you’re looking for a miracle, keep scrolling. 😑
Caroline Johnson
18 January 2026!!! THIS DRUG IS OVERHYPED!!!; THE MARKETING MACHINE IS PUSHING IT LIKE A BEACON, BUT THE REALITY IS THAT MANY PATIENTS END UP DEALING WITH UTI’S, DEHYDRATION, AND EVEN KETOACIDOSIS!!!; IF YOU’RE NOT READY TO MONITOR YOUR BODY CONSTANTLY, STEER CLEAR!!!;
Sumeet Kumar
27 January 2026Great discussion here! 🌟 It’s encouraging to see both the benefits and the cautions laid out so clearly. For anyone considering Forxiga, remember to stay hydrated, keep an eye on any unusual symptoms, and keep the dialogue open with your healthcare team. Together we can make informed choices and stay ahead of the curve! 🚀
Maribeth Cory
5 February 2026Let’s keep the conversation supportive and evidence‑driven. If you’ve tried Forxiga and had a positive experience, share what worked for you-diet tweaks, monitoring tips, or coping strategies for the minor side effects. Likewise, if you faced challenges, your insights can help others navigate the same path. We’re all in this together, and collective knowledge empowers us to manage diabetes more effectively.