Depigmentation Option Comparison Tool
Treatment Comparison
| Feature | Selected Treatment | Comparison Treatment |
|---|---|---|
| Mechanism | - | - |
| Typical Duration | - | - |
| Effectiveness | - | - |
| Side Effects | - | - |
| Cost (USD) | - | - |
| Availability | - | - |
Quick Decision Guide
Tip: For extensive stable vitiligo patches, consider Benoquin for permanent lightening. For mild cases or reversibility, hydroquinone or corticosteroids may be better choices.
When it comes to permanent skin depigmentation, especially for vitiligo patches that won’t respond to other therapies, the market offers a handful of options-some chemical, some procedural. Benoquin Cream is a topical monobenzone formulation that promises lasting loss of pigment by targeting melanocytes directly. But does it truly outperform the alternatives, or are there hidden trade‑offs? Below is a straight‑talk, side‑by‑side look at the most common rivals, plus practical tips for choosing the right route.
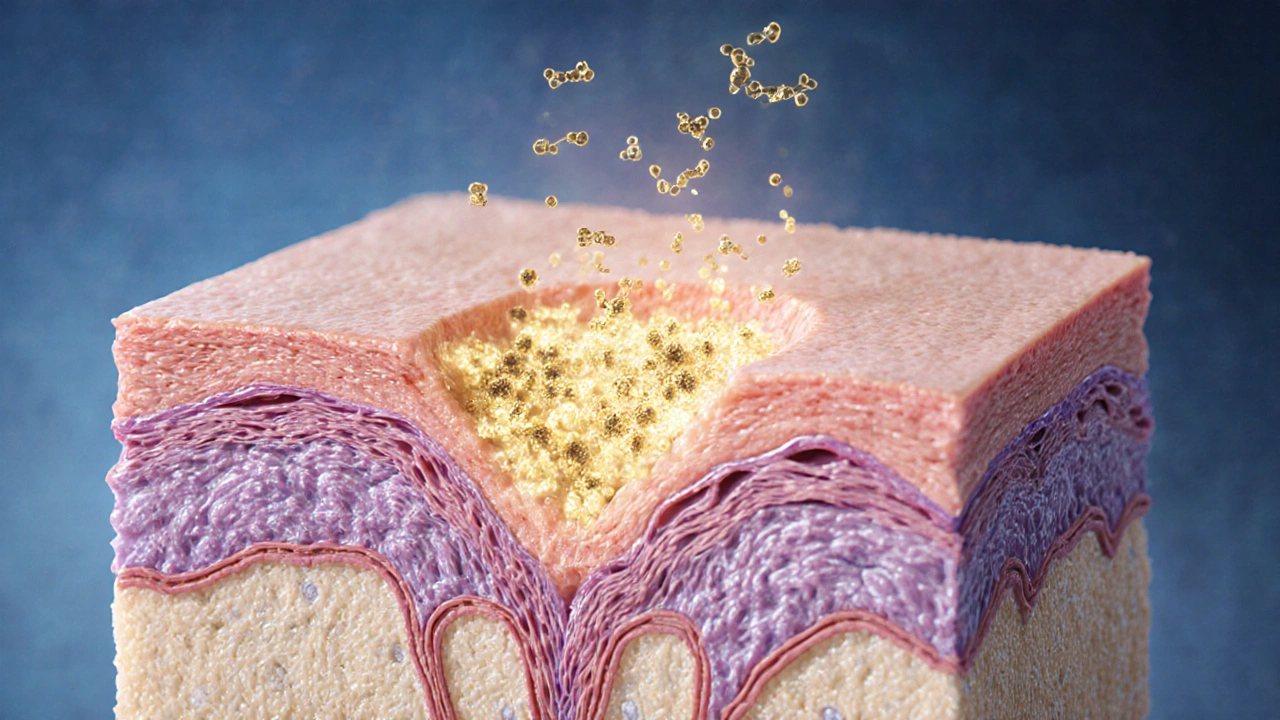
How Benoquin Cream Works
Monobenzone (the active ingredient in Benoquin Cream) binds to melanin and chemically destroys melanocytes, the cells that produce pigment. The effect is irreversible-once a patch is lightened, it stays that way for life. Treatment usually starts with a low‑dose test area, then ramps up to twice‑daily applications for several months. Most users notice noticeable lightening after 8‑12 weeks, with full effect around 6‑12 months.
Key Alternatives at a Glance
Here’s a quick snapshot of the most frequently mentioned substitutes. Each has a different mechanism, timeline, and safety profile.
| Option | Mechanism | Typical Duration | Effectiveness | Common Side Effects | Cost (USD) | Availability |
|---|---|---|---|---|---|---|
| Benoquin Cream (Monobenzone) | Melanocyte cytotoxicity | 6‑12months for full effect | 80‑90% permanent lightening | Contact dermatitis, temporary erythema | ≈$350‑$500 per 30g tube | Prescription (U.S., Canada, EU) |
| Hydroquinone Cream | Tyrosinase inhibition (reversible) | 3‑6months, maintenance needed | 30‑50% temporary lightening | Ochronosis, irritation | ≈$30‑$80 per 20g tube | OTC (≤2%) or prescription (≥4%) |
| Topical Corticosteroids | Anti‑inflammatory, melanocyte suppression | 4‑8weeks per course | 10‑20% modest lightening | Skin thinning, telangiectasia | ≈$15‑$40 per tube | Prescription |
| Tretinoin (Retinoic Acid) | Accelerates turnover, melanin dispersion | 6‑12months, combined with other agents | 15‑25% when combined | Peeling, dryness | ≈$20‑$60 per 20g tube | Prescription |
| Laser Therapy (Q‑switched) | Selective photothermolysis of melanin | Multiple sessions over 6‑12months | 50‑70% reduction (often temporary) | Post‑inflammatory hyperpigmentation, scarring | ≈$1,200‑$3,000 total | Professional clinic |
| Surgical Skin Grafting | Transplantation of pigmented skin | Single procedure, healing 2‑4weeks | 75‑85% match, permanent if graft holds | Donor site scarring, graft rejection | ≈$4,000‑$8,000 per area | Specialized surgical center |
When Benoquin Cream Makes Sense
If you’ve tried reversible agents like hydroquinone or steroids and the results faded as soon as you stopped, Benoquin offers a one‑time commitment for lasting change. It shines in these scenarios:
- Extensive vitiligo patches that are stable (no active spreading).
- Patients who prefer a non‑procedural route over laser or surgery.
- Those willing to manage occasional mild irritation for a permanent outcome.
Because the pigment loss is irreversible, a test spot is crucial. Most dermatologists recommend a 2‑week trial on a discreet area before committing to full‑body use.
Drawbacks to Keep in Mind
Permanent isn’t always a perk. Once your skin loses melanin, you lose natural UV protection in that area. That means you’ll need diligent sunscreen use-SPF30+broad‑spectrum-every day, even in winter. Some users report a burning sensation during the first weeks, and a small percentage develop contact dermatitis that requires a short course of steroids.
Regulatory-wise, Benoquin is not FDA‑approved in the United States (it’s considered a compounding prescription) but is available in Canada, Europe, and a few Asian markets under strict medical supervision.
How the Alternatives Stack Up
Every alternative has its own sweet spot. Hydroquinone, for example, works well for mild hyperpigmentation (age spots, melasma) but can cause ochronosis with long‑term use. Corticosteroids are great for inflammation‑driven depigmentation but risk skin atrophy if used beyond a few weeks.
Tretinoin shines when paired with other agents-its exfoliating action lets other compounds reach melanocytes more effectively. Laser therapy provides quick visual results, yet the effect can fade if the underlying autoimmune process remains active. Surgical grafting delivers a perfect color match but demands a skilled surgeon and carries the usual risks of any operation.
Cost‑Benefit Quick Guide
Let’s break down the money side. Benoquin’s upfront price looks steep, but when you compare it to the cumulative cost of multiple laser sessions or repeated purchases of hydroquinone creams, the gap narrows. For a typical 30g tube, you’re looking at $350‑$500, which usually covers 6‑12months of treatment. Laser packages can easily top $2,000, and grafting runs into the thousands per treated area.
Insurance rarely covers Benoquin or laser because they’re deemed cosmetic in many regions. However, some private health plans in Canada may reimburse a portion if a dermatologist writes a medical necessity letter.

Practical Decision Tree
- Is your vitiligo stable for at least 6months? Yes → Consider Benoquin or laser.
- Do you prefer a non‑invasive, at‑home regimen? Yes → Benoquin or hydroquinone (if reversible is okay).
- Are you comfortable with possible skin irritation and need for strict sun protection? Yes → Benoquin.
- Do you have a budget under $1,000? Yes → Hydroquinone, corticosteroids, or tretinoin combos.
- Is permanent pigment loss a must‑have? Yes → Benoquin (or surgical grafting if you want natural pigment).
Following this flow helps you land on the option that fits your lifestyle, risk tolerance, and wallet.
Tips for Using Benoquin Safely
- Start with a 2% concentration on a small patch for 2‑3weeks.
- Apply twice daily, avoiding broken skin.
- Use a fragrance‑free moisturizer to counter dryness.
- Apply broad‑spectrum sunscreen (SPF30+) on treated areas each morning.
- Schedule monthly follow‑ups with your dermatologist to monitor progress and side effects.
Frequently Asked Questions
Can Benoquin Cream be used on children?
Most dermatologists advise against using monobenzone on patients under 12years old because their skin is more sensitive and long‑term effects are less studied. In rare cases, a specialist may prescribe a very low dose with close monitoring.
How long does the lightening effect last after stopping Benoquin?
The pigment loss is considered permanent. Stopping the cream will not bring back the original color, but you must continue using sunscreen to protect the newly unpigmented skin.
Is there a risk of allergic reaction?
Yes, about 5‑10% of users develop contact dermatitis. If you notice redness, itching, or burning that doesn’t subside in a few days, stop the cream and consult a dermatologist for a steroid rinse.
How does Benoquin compare to laser therapy in terms of safety?
Benoquin avoids the risk of burns, scarring, or post‑inflammatory hyperpigmentation that can accompany laser sessions. However, it does require strict sun avoidance, while lasers can be performed on already protected skin.
Can I combine Benoquin with other depigmenting agents?
Combining monobenzone with other topical agents isn’t generally recommended because the skin barrier is already stressed. If additional lightening is needed, doctors may add a short course of tretinoin after the monobenzone phase.
Choosing the right depigmentation strategy is personal. By weighing permanence, side‑effects, cost, and convenience, you can decide whether Benoquin Cream comparison points you toward monobenzone or another route. Whichever path you take, a dermatologist’s guidance and diligent sun protection are non‑negotiable for the best outcome.







Comments
Mark Quintana
7 October 2025Got the gist, looks solid.
Brandon Cassidy
7 October 2025Reading through the comparison, the permanence of monobenzone stands out.
The trade‑off with sun protection is something to keep in mind.
Taylor Yokum
7 October 2025The table does a good job of laying out the basics in plain language.
For anyone new to skin depigmentation, it’s a helpful starting point.
Just remember that individual response can vary a lot, so a dermatologist’s guidance is still key.
Taryn Esses
7 October 2025Interesting breakdown.
Albert Lopez
7 October 2025The author’s exposition of monobenzone’s mechanism is technically accurate, yet it omits the nuanced pharmacokinetics that influence cutaneous distribution.
A thorough analysis would consider the drug’s lipophilicity and its propensity to accumulate in the stratum corneum.
Furthermore, the comparison table fails to address the heterogeneity of vitiligo pathogenesis, which renders a one‑size‑fits‑all recommendation imprudent.
Clinical studies cited suggest an 80‑90 % depigmentation rate, but these figures derive from small cohort trials lacking long‑term follow‑up.
The absence of data on post‑treatment melanoma surveillance is a glaring oversight, given the loss of melanin’s protective function.
Cost considerations, while superficially presented, neglect the ancillary expenses of lifelong photoprotection.
Patients may also incur periodic dermatologic visits to monitor for contact dermatitis, a factor not quantified in the presented financial summary.
Comparatively, laser therapy’s transient efficacy is juxtaposed against a higher incidence of post‑inflammatory hyperpigmentation, a point the article underrepresents.
Surgical grafting, though invasive, offers a potential for permanent pigment restoration, but the risk of graft rejection is understated.
The author’s recommendation algorithm assumes stability of disease for six months, yet does not advise confirmatory auto‑immune markers.
Moreover, the lack of discussion regarding off‑label usage in jurisdictions where monobenzone is not approved raises ethical concerns.
From a regulatory standpoint, the assertion that Benoquin is merely a prescription medication obscures its compounding nature in the United States.
The safety profile outlined omits the rare but documented cases of Stevens‑Johnson‑like reactions.
In sum, while the article provides a useful snapshot, the depth of analysis required for informed consent is insufficient.
Prospective users would benefit from a more exhaustive risk‑benefit matrix before committing to irreversible depigmentation.
Halle Redick
7 October 2025That’s a solid critique, thanks for laying it out. It really helps anyone weighing the pros and cons.
Erica Harrington
7 October 2025For folks on the fence, remember that each treatment path comes with its own set of trade‑offs, but staying informed is the first step toward a confident decision.
Keep the dialogue open with your dermatologist, and don’t shy away from asking about long‑term follow‑up plans.
Your skin’s future is worth the extra conversation.
Patricia Mombourquette
7 October 2025Facts over fluff.
karl lewis
7 October 2025The comparative analysis, while visually appealing, suffers from a paucity of primary literature citations.
One cannot accept the asserted superiority of monobenzone without rigorous randomized controlled trials.
The author neglects to discuss the pharmacodynamic variability among patients of differing Fitzpatrick skin types.
Furthermore, the economic evaluation fails to incorporate indirect costs such as lost productivity due to treatment‑related adverse events.
The omission of a systematic review methodology renders the presented data anecdotal at best.
A prudent clinician would demand meta‑analytic evidence before endorsing irreversible depigmentation.
The article’s brief mention of sunscreen compliance glosses over the well‑documented increase in photodermatoses among depigmented skin.
It is also noteworthy that the regulatory status of monobenzone varies dramatically across jurisdictions, a point the author glosses over.
The safety section does not address the potential for systemic absorption leading to off‑target effects.
In contrast, laser therapy, despite its higher upfront cost, offers the advantage of reversible outcomes pending parameter adjustments.
Surgical grafting, albeit invasive, is supported by a modest body of literature demonstrating durable pigment normalization.
The decision algorithm presented lacks weighting for patient quality‑of‑life metrics, an oversight of ethical significance.
Moreover, the discussion of side‑effect profiles is superficial, ignoring the psychological impact of treatment‑induced scarring.
The recommendation to initiate monobenzone on a test patch is sound, yet the duration of observation is inadequately defined.
Overall, the piece would benefit from a more exhaustive and evidence‑based approach before serving as a clinical guide.
Amy Martinez
7 October 2025Wow, that’s a thorough dissection, and I appreciate the depth. It’s like you’ve peeled back every layer of the onion to reveal the core concerns. Let’s hope future articles take that level of rigor.
Josh Grabenstein
7 October 2025Sure, but you’re all missing the bigger picture – pharma loves these "options" 🤔