When your pharmacist hands you a pill that looks completely different from what you’ve been taking, it’s normal to feel uneasy. Maybe it’s a smaller white tablet instead of a large blue capsule. Maybe the name on the bottle is unfamiliar. You might wonder: Is this really the same thing? The answer is yes - most of the time. But not always. And knowing when to expect trouble can save you from serious side effects or treatment failure.
Generic drugs are not knockoffs - they’re FDA-approved copies
Generic drugs contain the exact same active ingredient, in the same strength, and work the same way in your body as the brand-name version. The FDA requires them to meet the same strict standards for quality, safety, and effectiveness. In fact, the same factories sometimes make both the brand and the generic version - just under different labels. The difference isn’t in what heals you; it’s in what holds it together.Brand-name drugs get their name because the company that invented them paid millions to develop, test, and market them. Once their patent expires (usually after 20 years), other companies can make copies. These copies are called generics. They don’t need to repeat expensive clinical trials because the original drug’s safety and effectiveness are already proven. Instead, they must prove they deliver the same amount of medicine into your bloodstream at the same rate. That’s called bioequivalence. The FDA requires generics to stay within 80% to 125% of the brand’s absorption levels - a very tight window. Real-world data shows most generics actually vary by less than 5%.
You’ll save money - a lot of it
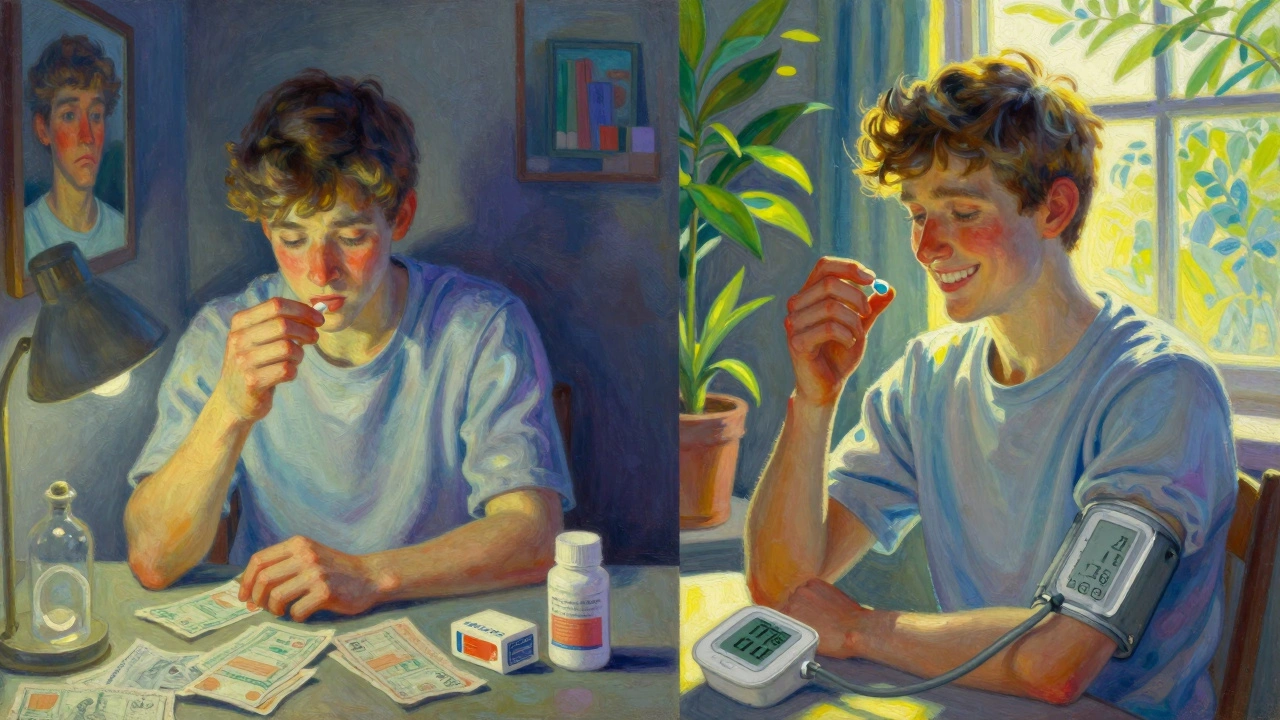
The biggest reason to switch is cost. On average, generic drugs cost 80% to 85% less than brand-name versions. For example, if your brand-name cholesterol pill costs $350 a month, the generic might cost $15. That’s not a small difference - it’s the difference between taking your medicine every day or skipping doses because you can’t afford it.According to the Centers for Medicare & Medicaid Services, patients who switch to generics save an average of $378 per prescription each year. For people on multiple medications, that adds up to thousands. Medicare Part D beneficiaries save about $1,268 annually just by using generics instead of brands. And it’s not just for seniors - people with private insurance see the same savings at the pharmacy counter.
One patient in Phoenix told ABC15 she was skipping her cholesterol meds because they cost $350 a month. After switching to the generic - $15 - she started taking them regularly. Her cholesterol dropped. Her doctor was impressed. That’s the real impact: affordability leads to adherence, and adherence saves lives.
What’s different? Appearance and fillers - not the medicine
Generics look different because U.S. trademark laws require them to. You can’t copy the exact color, shape, or logo of a brand-name drug. So a blue oval pill might become a white round tablet. A capsule might turn into a tablet. That’s not a sign of lower quality - it’s a legal requirement.But here’s what matters more: the inactive ingredients. These are the fillers, dyes, binders, and preservatives that hold the pill together. They don’t treat your condition, but they can cause problems if you’re allergic. For example, some generics use red dye (FD&C Red No. 40), which can trigger reactions in sensitive people. Others use lactose, which can upset those with severe lactose intolerance. The FDA requires manufacturers to list these ingredients on the patient package insert - but not always clearly. A 2022 University of Michigan study found only 37% of generic labels clearly warn about common allergens.
If you’ve had allergic reactions to medications before, always check the inactive ingredients. Ask your pharmacist for the full list. Don’t assume it’s the same as the brand. And if you notice new rashes, swelling, or stomach upset after switching, report it.
When switching might cause problems
Most of the time, switching to a generic works perfectly. But there are exceptions. The FDA calls them narrow therapeutic index (NTI) drugs. These are medications where even tiny changes in blood levels can cause big problems - either the drug stops working or it becomes toxic.Examples include:
- Levothyroxine (for hypothyroidism)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
A 2021 study by the American Epilepsy Society found that 12.7% of patients switching between different generic versions of antiseizure drugs had breakthrough seizures. That’s nearly three times higher than patients who stayed on one formulation. Some neurologists now recommend sticking with the same generic manufacturer - or even the brand - if you’ve been stable.
Same goes for warfarin. A shift in INR levels - even by 0.5 - can increase your risk of clotting or bleeding. If you’re on warfarin, your doctor will likely monitor your blood more closely after a switch.
Another area where generics can struggle: complex delivery systems. Inhalers, patches, and eye drops rely on precise physical properties to work. A 2020 FDA warning noted that some generic versions of Advair Diskus didn’t disperse the powder the same way, leading to inconsistent dosing. These aren’t common yet, but they’re growing.
What to do when you switch
You don’t need to panic when you get a new pill. But you should be smart about it.Step 1: Ask your pharmacist - “Is this the generic version of my brand? What’s different?” They’re required to give you a 5-7 minute counseling session in most states. Use it.
Step 2: Check the label - Look for the patient package insert. It lists all inactive ingredients. If you see something you’re allergic to, call your doctor before taking it.
Step 3: Track your symptoms - For the first two weeks, keep a simple log. Note:
- Any new side effects (dizziness, nausea, rash)
- Changes in how you feel (more tired, less pain, mood shifts)
- For specific conditions: blood sugar levels (diabetes), INR numbers (warfarin), seizure frequency, or depression scores (PHQ-9)
Step 4: Don’t assume all generics are the same - Two different companies can make generics for the same drug. One might work better for you than the other. If you switch from one generic to another and feel worse, tell your doctor. You may need to stick with the one that worked.

When you should avoid switching
There are times when staying on the brand is the safer choice:- You’ve had a bad reaction to a generic before
- You’re on an NTI drug and your condition is unstable
- Your doctor specifically says not to switch (some specialists do this for epilepsy, transplant, or psychiatric meds)
- You’re using a complex delivery system like an inhaler or patch, and you’ve noticed changes in how it works
Even then, it’s worth asking: “Is there a generic version that’s been proven equivalent for my condition?” Sometimes, newer generics have improved. Don’t accept “no” without a second opinion.
What’s changing in 2025
The FDA is pushing for better labeling. By 2025, all generic drug packaging must clearly list potential allergens - no more hiding them in fine print. The Inflation Reduction Act also means Medicare will cover all approved generics without prior authorization starting in 2024, making it even easier to switch.More complex generics are coming too - like orally disintegrating tablets, extended-release capsules, and transdermal patches. These are harder to copy, but manufacturers are getting better. By 2024, over 200 new generic approvals are expected, including biosimilars for expensive biologics like Humira.
Meanwhile, the generic drug market is growing. In 2023, generics made up 90% of all prescriptions filled in the U.S. - but only 20% of total drug spending. That’s because they’re cheap. And as more patents expire, that number will keep rising. The Congressional Budget Office predicts 95% of prescriptions will be generic by 2030.
Bottom line: Trust the science, but stay alert
Generic drugs are safe, effective, and life-changing for millions. They’re not inferior. They’re just more affordable. For most people, switching means better health - not worse.But your body is unique. If you feel different after a switch, don’t ignore it. Track it. Talk to your doctor or pharmacist. You’re not being difficult - you’re being responsible.
And if cost is keeping you from taking your medicine? The generic is your answer. Millions have made the switch and kept their health intact. You can too.
Are generic drugs as effective as brand-name drugs?
Yes, for the vast majority of medications. The FDA requires generics to prove they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. Studies show generics work the same as brands in about 88% of cases. The only exceptions are drugs with a narrow therapeutic index - like warfarin, levothyroxine, and certain seizure medications - where small changes can matter.
Why do generic pills look different?
U.S. trademark laws prevent generic drugs from looking identical to brand-name drugs. That means the color, shape, size, or imprint may be different. This has nothing to do with effectiveness - it’s just a legal requirement. The active ingredient is still the same.
Can generic drugs cause new side effects?
Rarely, but yes. The active ingredient is the same, but the inactive ingredients (like dyes, fillers, or preservatives) can differ. If you’re allergic to lactose, red dye, or gluten, a new generic might trigger a reaction you didn’t have before. Always check the patient package insert for inactive ingredients when you get a new prescription.
Should I always choose the cheapest generic?
Not always. Different manufacturers make generics, and sometimes one works better for you than another. If you switch from one generic to another and feel worse, tell your doctor. You may need to stick with the specific brand or generic version that works best for you. Your pharmacist can help track which manufacturer you’ve used.
How do I know if my generic is FDA-approved?
All legally sold generics in the U.S. must be FDA-approved. You can check the FDA’s Orange Book online - it lists all approved generic equivalents. But you don’t need to do that yourself. Your pharmacist knows. If your pharmacy is licensed and reputable, you can trust the generic they dispense.
Is it safe to switch between different generic brands?
For most drugs, yes. But for narrow therapeutic index medications like levothyroxine or antiseizure drugs, switching between manufacturers can cause problems. If you’re on one of these drugs, ask your doctor if you should stick with the same manufacturer. Some patients do better with one brand of generic than another - even if both are FDA-approved.
What if I can’t afford my brand-name drug?
Switching to the generic is your best option. Skipping doses because of cost is dangerous. For example, people on statins who skip doses because of price have a much higher risk of heart attack. Generics cost 80-85% less. Many patients report improved adherence and better health after switching. If even the generic is too expensive, ask your pharmacist about patient assistance programs or discount cards like GoodRx.







Comments
Kumar Shubhranshu
7 December 2025Generic works fine for me
Ibrahim Yakubu
7 December 2025You think it's that simple? In Nigeria we've seen generics that turn into dust in your hand. FDA? That's a US thing. Who's checking these pills in Lagos? Some of these generics are just sugar pills with a fancy label. Don't be fooled.
Andrew Frazier
8 December 2025Wow. So you're telling me I should trust some factory in India that doesn't even speak English to make my heart medicine? I paid for brand because I want quality. Not some cheap knockoff made by guys who can't spell 'pharmaceutical'. This is why America's healthcare is falling apart.
olive ashley
9 December 2025They're watching you. The pharmaceutical cartel lets generics in so they can track your blood levels. Every time you switch, they log it. Next thing you know, your insurance hikes your premiums because 'your body is unstable'. I read it on a forum. It's all connected.
Mayur Panchamia
9 December 2025Ohhhhh, so now we're trusting the FDA?? The same agency that let OxyContin through?? The same ones who approved 37 different versions of Adderall that all work differently?? You're a fool if you think this is about safety-it's about PROFITS. The big boys want you hooked on $350 pills so they can keep raking in billions while you beg for coupons. Generics? They're the only real rebellion left.
Myles White
9 December 2025I've been on levothyroxine for 12 years and I've switched generics three times. First time, I got super anxious and my heart raced. Second time, I felt like I was walking through molasses. Third time, I stuck with the same manufacturer-Sandoz-and everything stabilized. It's not about brand vs generic, it's about consistency. If your doctor doesn't know this, find a new one. Also, the inactive ingredients matter more than people admit. I'm lactose intolerant and I didn't realize until I got a rash after a new generic. Always check the insert. Always.
brenda olvera
11 December 2025My mom switched to generic blood pressure meds and she's never felt better. She said she didn't even notice the difference until she saw the price. Now she takes them every day. That's what matters. Health isn't about labels. It's about showing up for yourself. And generics help you do that. So much love to everyone who's choosing to live instead of skipping doses because of cost
Priya Ranjan
12 December 2025Anyone who says generics are 'just as good' hasn't lived with a seizure disorder. My cousin went from zero seizures on brand to three in a week after switching. The neurologist said it was 'within FDA limits'-but what good is that when your cousin is in the ER? You don't gamble with your brain. Some people are fine. Others aren't. Stop pretending it's one-size-fits-all.
Nava Jothy
14 December 2025Oh my GOD. I switched to a generic antidepressant last year and I cried for three days straight. I thought I was going crazy. Turns out the dye was triggering my anxiety. I almost lost my job. My therapist said I was 'overreacting.' But I wasn't. My body knew. I'm so tired of people acting like side effects are 'in your head.' If you feel different, you ARE different. And if your doctor dismisses you? Find someone who listens. I'm still healing. 💔
Chris Park
16 December 2025Interesting how the article ignores the fact that the FDA's bioequivalence standard of 80-125% is a 45% swing. That's not 'tight'-that's a legal loophole. A drug can be 45% weaker or stronger and still be approved. In real life, that's not medicine, that's Russian roulette. And don't get me started on the fact that the same company that makes the brand also makes the generic. It's not competition-it's collusion. The whole system is rigged. You're not getting savings-you're getting a gamble.