Every year, Americans spend over $700 billion on prescription drugs. But here’s the twist: 90% of all prescriptions filled are for generic medicines - and they cost just 12% of what brand-name drugs do. That’s not a coincidence. It’s the single biggest reason the U.S. healthcare system hasn’t collapsed under its own weight.
What’s Really Going On With Drug Prices?
In 2024, 3.9 billion prescriptions were filled in the U.S. Nearly all of them - 9 out of 10 - were generics. Yet those generics only accounted for $98 billion in total spending. Meanwhile, brand-name drugs made up just 10% of prescriptions but swallowed up $700 billion. That means generics saved the system $482 billion in one year alone. That’s more than the entire annual budget of the Department of Education. This isn’t new. Since 2016, generics have consistently made up 90% of prescriptions. But here’s what’s changed: their share of total spending has dropped from 27% to 12%. Why? Because manufacturers are producing more generics, and competition is driving prices down. Even though more people are using them, the cost per pill keeps falling. That’s the opposite of what happens with most other goods.How Do Generics Actually Save Money?
Generic drugs aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to recoup billions in research and marketing costs. When a brand-name drug’s patent expires, other companies can make the exact same medicine. The FDA requires generics to be bioequivalent - meaning they work the same way in your body. No shortcuts. No compromises. Take albuterol, the inhaler used for asthma. The brand version can cost $60 per refill. The generic? Around $10. That’s an 83% drop. One Reddit user in the r/Pharmacy subreddit said switching to generic albuterol saved them $300 a month. For someone living paycheck to paycheck, that’s not just savings - it’s survival. The same math applies to blood pressure pills, cholesterol meds, diabetes drugs. If you’re on a monthly prescription, going generic can cut your out-of-pocket cost by half or more. And it’s not just individuals. Health plans, Medicare, and employers save billions because they’re paying less per prescription. CMS data shows that less than 1% of Medicare beneficiaries hitting catastrophic coverage use only brand-name drugs. Why? Because they can’t afford to.The Biosimilar Revolution
Biosimilars are the next wave. They’re not exact copies like traditional generics - they’re highly similar versions of complex biologic drugs made from living cells. Think Humira, Stelara, or insulin. These drugs used to cost $70,000 a year. Now, with biosimilars entering the market, prices are dropping by 80% or more. In 2024, Humira biosimilar use jumped from 3% to 28% in just one year after health plans started pushing them. That single shift saved billions. Stelara, a $6 billion drug, now has seven FDA-approved biosimilars ready to launch. Once fully adopted, those biosimilars could save $4.8 billion annually. But here’s the problem: 90% of the biologics set to lose patent protection in the next 10 years have no biosimilar in development. That’s a $234 billion missed opportunity. Why? Because big pharma uses legal tricks to delay competition. They pay generic makers to wait - a practice called “pay for delay.” In 2024, brand-name companies spent $1.2 billion on these settlements. That’s money taken directly from patient wallets.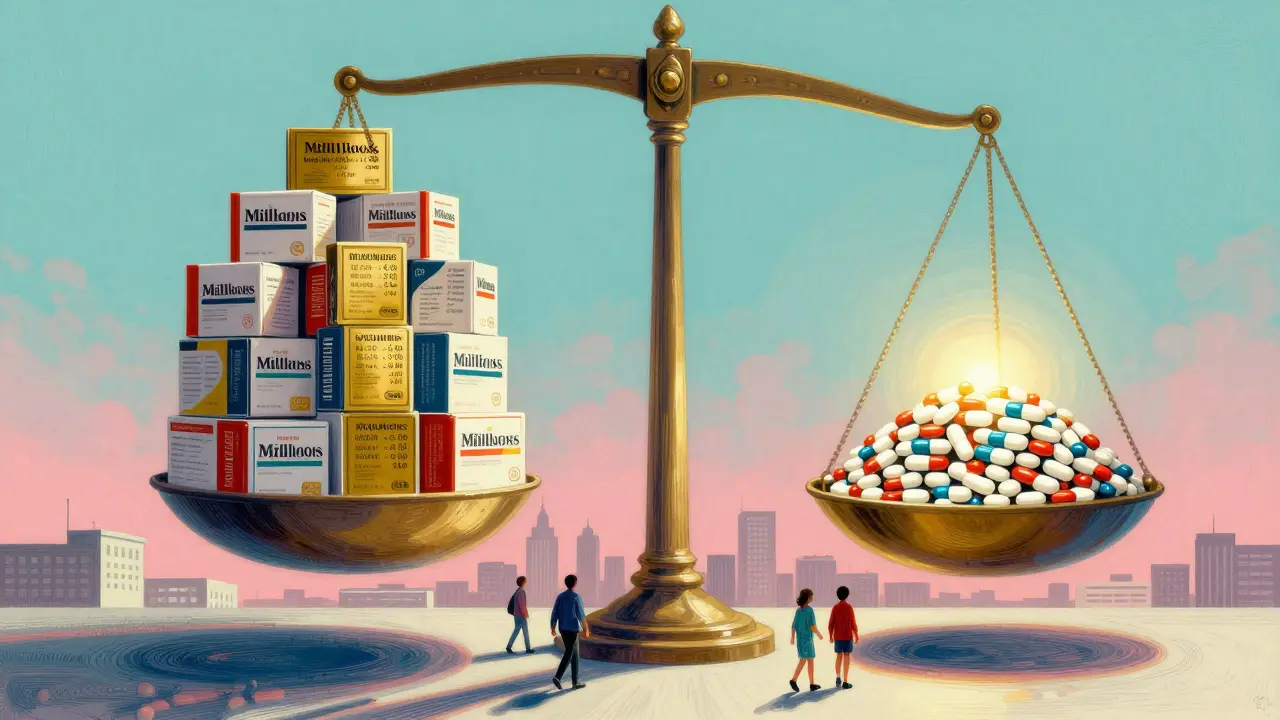
Why Are Brand-Name Drugs So Expensive?
The U.S. pays more than three times what other developed countries pay for the same brand-name drugs. Why? Because we don’t negotiate prices. Medicare couldn’t negotiate drug prices until 2022, and even now, only 10 drugs are covered under the new program. The Inflation Reduction Act changed that - but slowly. By 2026, Medicare will negotiate 30 drugs a year. If that expands to Medicaid and private insurance, the Congressional Budget Office estimates $1 trillion in savings over a decade. Look at insulin. In 2023, Eli Lilly’s insulin cost $275 per vial. After public pressure and Medicare’s $35 cap, they dropped it to $25. That’s not because manufacturing got cheaper. It’s because people fought back. The same thing happened with Ozempic and Wegovy. After the White House struck deals with Eli Lilly and Novo Nordisk, those drugs dropped from over $1,000 to $350 per month. This proves one thing: drug prices aren’t set by science. They’re set by power.Who Benefits From Generic Drugs?
Everyone. Patients pay less. Insurers pay less. Employers pay less. Taxpayers pay less. Even hospitals save money because they’re not stuck with sky-high drug bills. The generic drug industry supports 350,000 jobs across 46 states. It’s not just pharmacies and clinics - it’s manufacturing plants, logistics hubs, quality control labs. It’s a real economy built on affordable medicine. But here’s the irony: the people who need generics most - low-income families, seniors on fixed incomes, people with chronic conditions - are often the ones facing the biggest barriers. Pharmacists sometimes switch between different generic brands without telling you. One person’s generic metformin might work perfectly. Another’s might cause stomach issues because of different fillers. That’s not the fault of generics. It’s the fault of a system that doesn’t track or regulate those differences.
What’s Holding Back More Savings?
We have the tools. We have the data. We know generics and biosimilars work. So why aren’t we using them more? First, insurance plans and pharmacy benefit managers (PBMs) often don’t incentivize switching. They make more money when you stay on expensive brand drugs. Second, doctors still default to prescribing brand names because they’re familiar with them - or because reps visit their offices with free samples. Third, patients are scared. They’ve been told generics are “weaker” or “not as good.” That myth needs to die. The solution? Clear rules. Health plans should require generics unless there’s a medical reason not to. Pharmacists should be trained to explain the equivalence. Patients should be given a choice - not a surprise substitution.The Future Is Affordable
By 2030, if current trends continue, generic and biosimilar use could cut U.S. prescription drug spending by 15-18%. That’s $100+ billion in annual savings. If we fix the biosimilar void - if we stop letting pharma delay competition - we could save another $234 billion over the next decade. The system isn’t broken. It’s being manipulated. Generic drugs are the most effective, proven, and underused tool we have to fix it. They don’t need new laws. They need enforcement. They need transparency. They need patients and providers to demand them. You don’t need to wait for Washington to act. Ask your doctor: “Is there a generic?” Ask your pharmacist: “Can I get the lowest-cost version?” Ask your insurer: “Why am I paying more for the same medicine?” The savings are real. The science is solid. The only thing missing is the will to use it.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body. In fact, many generics are made in the same factories as brand-name drugs. The only differences are in inactive ingredients like fillers or dyes - which rarely affect how the drug works.
Why do some people say generics don’t work for them?
Sometimes, switching between different generic versions - even if they’re both approved - can cause minor side effects because of differences in inactive ingredients. For example, one generic metformin might have a different binder that causes stomach upset for some people. This isn’t about effectiveness - it’s about individual tolerance. If you notice a change after switching, talk to your pharmacist. They can often switch you back to the same generic brand you used before.
Do biosimilars cost less than brand-name biologics?
Yes - often by 80% or more. For example, Humira biosimilars launched at about $1,500 per month, while the original cost over $7,000. That’s a 78% drop. The same pattern holds for Stelara, Enbrel, and insulin. Once multiple biosimilars enter the market, prices drop even further due to competition. Health plans that actively promote biosimilars have seen their drug spending fall by double digits in just one year.
Why don’t doctors always prescribe generics?
Some doctors aren’t aware of available generics, especially for newer conditions. Others are influenced by pharmaceutical reps who push brand-name drugs with free samples or educational materials. In some cases, insurance plans don’t make generics the default option. But the biggest reason? Habit. Many prescribers stick with what they know. Patients can help by asking, “Is there a generic version?” - and making it clear they want the lowest-cost option that works.
Can I trust generics from foreign countries?
The FDA inspects all generic drug manufacturing facilities - whether they’re in the U.S., India, or China - before approving them. Over 80% of generic drugs sold in the U.S. are made overseas, and they’re held to the same standards as U.S.-made drugs. The real risk isn’t where they’re made - it’s buying from unregulated online pharmacies. Always get your meds from licensed U.S. pharmacies. If a price seems too good to be true, it probably is.
How do I know if my insurance covers a generic?
Check your plan’s formulary - the list of covered drugs. Most insurers have a tiered system where generics are in the lowest tier, meaning you pay the least. You can usually find this online through your insurer’s website or app. If your prescription is expensive, ask your pharmacist to check for alternatives. Many pharmacies have apps that show real-time prices at different locations - sometimes the cash price for a generic is lower than your copay.
What’s the biggest barrier to more generic drug savings?
The biggest barrier is deliberate delay. Big pharma spends billions to block competition - through patent extensions, lawsuits, and “pay for delay” deals. These tactics keep prices high even after patents expire. Until we enforce antitrust laws and stop these practices, savings will remain limited. The public doesn’t see these deals - but they feel the impact in higher premiums and out-of-pocket costs.







Comments
bhushan telavane
20 December 2025Back home in India, generics are the only option for most people. We don't have a choice, so we trust them. Saw my uncle switch from brand insulin to generic and his HbA1c stayed the same. Same pill, same results, 90% cheaper. Why is this even a debate?
Mahammad Muradov
20 December 2025Let me be clear. The FDA’s bioequivalence standards are a joke. They allow 80-125% variability in absorption. That’s not ‘the same’-that’s a lottery. People get sick because they’re handed different generics every month. This isn’t saving money-it’s gambling with health.
Connie Zehner
20 December 2025OMG I’m so mad!! 😭 I got switched to a generic metformin last month and I felt like I was gonna vomit for two weeks. My pharmacist didn’t even tell me it changed! This system is literally trying to kill us. #GenericFail
holly Sinclair
21 December 2025What’s fascinating here isn’t just the cost difference-it’s the philosophical shift in how we value medicine. We treat drugs like luxury goods, when they’re fundamentally public health infrastructure. The fact that we allow patent monopolies to dictate survival, while other nations negotiate as a collective, reveals a moral failure in our system. Generics aren’t just cheaper-they’re an act of justice.
Monte Pareek
22 December 2025If you're still paying full price for a brand-name drug when a generic exists you're either not trying or you're being manipulated. Ask your pharmacist for the lowest cost option. Always. Every time. Don't let them push you toward the expensive one. Your insurance doesn't care about your wallet. You have to care for them. And if your doctor doesn't know the generic? Educate them. You're not being rude-you're being smart
Tim Goodfellow
24 December 2025Generics are the unsung heroes of modern medicine. Like the quiet guy in the back who fixes the engine while everyone cheers the driver. No fanfare. No ads. Just pure, unglamorous, life-saving efficiency. And yet we treat them like second-class citizens. Time to give these heroes a parade
Elaine Douglass
25 December 2025I’ve been on generics for 12 years and never had an issue. My blood pressure is perfect. My cholesterol’s down. I just wish more people knew it’s okay to ask for the cheaper one. It’s not about being cheap-it’s about being smart
Alex Curran
25 December 2025My mate in Sydney got his asthma inhaler for $5 AUD through the PBS. Same generic as the US version. We don’t have the same pharma lobbying here. It’s not magic. It’s policy. We could do this too if we wanted to
Allison Pannabekcer
26 December 2025I get that some people have bad experiences with generics. But let’s not throw the baby out with the bathwater. The issue isn’t the drug-it’s the lack of tracking and communication. If pharmacies kept a log of which generic brand you responded to, and stuck with it, most side effects would vanish. It’s a system flaw, not a drug flaw
Sarah McQuillan
27 December 2025Let’s be real-this whole ‘generics save money’ thing is just woke corporate propaganda. Real Americans deserve the best, not some cheap knockoff made in China. If you can afford it, you should take the brand. That’s what freedom looks like
Aboobakar Muhammedali
28 December 2025My cousin in Delhi takes 7 different generics. One for heart one for sugar one for pain. He says if he had to pay brand prices he’d be dead. He never complains. He just takes his pills and thanks god for cheap medicine. We forget how lucky we are to even have access
Alana Koerts
30 December 202590% of prescriptions are generics? That’s not a win. That’s a failure of innovation. If we’re relying on 10-year-old chemistry just to survive then our healthcare system is on life support. The real problem isn’t price-it’s stagnation
Gloria Parraz
30 December 2025I work in a clinic and I see it every day. Patients cry when they find out their insulin is now $35. That’s not a policy win-that’s a moral emergency. We should be ashamed we ever let it cost $275. Generics aren’t the solution-they’re the bare minimum. And we’re still not giving everyone that
Sahil jassy
31 December 2025Bro just ask for the generic. It’s that simple. No drama. No stress. My dad’s on 5 generics. All work. All cheap. He laughs at people who pay extra. Just say the word and move on
Kathryn Featherstone
2 January 2026My mom switched to generic Lipitor and her cholesterol dropped even more than before. She didn’t know that could happen. Turns out sometimes the generic works better because the fillers are less irritating to her gut. It’s not one-size-fits-all. But it’s still medicine. And it’s still saving us