Vitamin D & Calcium Risk Calculator
Enter values and click Calculate to see your risk assessment
Risk Assessment Guide
- High Risk: Low vitamin D (<30 ng/mL) with low calcium (<8.5 mg/dL)
- Moderate Risk: Vitamin D between 20-30 ng/mL or calcium between 8.0-8.5 mg/dL
- Low Risk: Normal vitamin D (>30 ng/mL) and calcium (>8.5 mg/dL)
Key Takeaways
- Vitamin D helps the gut absorb calcium; without enough, blood calcium can drop.
- Low serum 25(OH)D (<20ng/mL) dramatically raises the risk of hypocalcemia.
- Older adults, people with limited sun, and those on certain meds are most vulnerable.
- Daily intake of 600-800IU for most adults, 1000-2000IU for high‑risk groups, keeps levels in the target range.
- Vitamin D3 (cholecalciferol) is more effective than D2 (ergocalciferol) for raising serum levels.
What Vitamin D is and why it matters
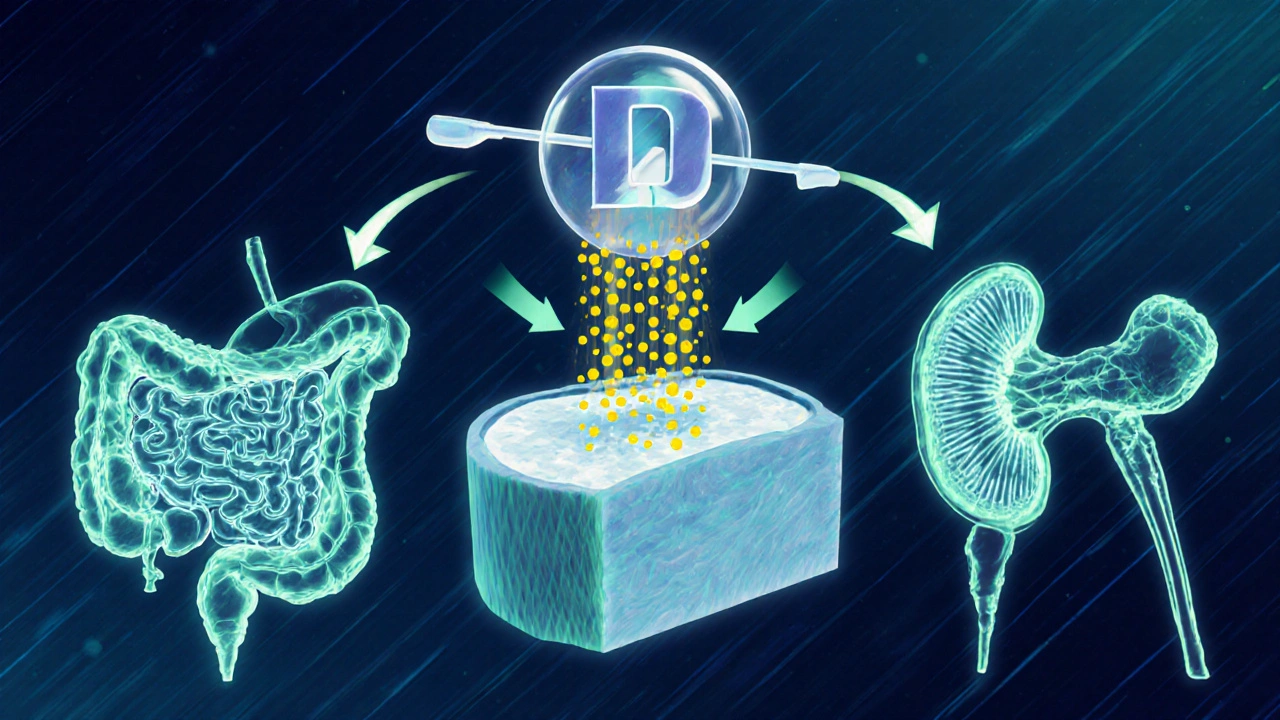
Often called the "sunshine vitamin," Vitamin D is a fat‑soluble nutrient that the body produces when skin is exposed to UV‑B radiation or is obtained from food and supplements. Its most active form, calcitriol, works like a hormone, directing the intestine, kidneys, and bones to manage calcium and phosphate.
When calcitriol signals the gut, calcium transport proteins are turned on, letting up to 40% of dietary calcium pass into the bloodstream. Without enough Vitamin D, that machinery stalls, and blood calcium levels can dip below the normal 8.5-10.2mg/dL range.
How Vitamin D prevents hypocalcemia a condition where blood calcium levels fall below the lower limit of normal, leading to muscle cramps, tingling, and in severe cases, cardiac arrhythmias
Calcium homeostasis is a three‑player game: the intestine (absorption), the bones (storage), and the kidneys (re‑absorption). Vitamin D is the conductor, ensuring each organ does its part. When Vitamin D levels drop, the intestine absorbs less calcium, the parathyroid glands release more parathyroid hormone (PTH) to compensate, and the kidneys try to reclaim calcium at the expense of phosphate.
Over time, the compensatory loop wears thin. PTH can keep serum calcium afloat, but only until bone stores are depleted, which can trigger osteomalacia or osteoporosis. The moment the system can’t keep up, hypocalcemia symptoms appear: tingling around the mouth, muscle spasms, and in extreme cases, seizures.
Who is most likely to run low on Vitamin D?
Even in sunny Toronto, many adults slip below the optimal serum 25(OH)D level. The following groups face the highest odds:
- Older adults: skin thins with age, producing less Vitamin D from the same sunlight.
- People with limited outdoor exposure: office workers, night‑shift staff, and residents of high‑latitude regions during winter.
- Individuals with darker skin: melanin absorbs UV‑B, reducing synthesis.
- Patients on certain medications: anticonvulsants, glucocorticoids, and some weight‑loss drugs increase Vitamin D metabolism.
- Those with malabsorption conditions: celiac disease, Crohn’s disease, and bariatric surgery can limit dietary uptake.
Blood tests that measure serum 25(OH)D the main circulating form of Vitamin D used to assess nutritional status are the gold standard. Levels under 20ng/mL signal deficiency, 20‑30ng/mL borderline, and 30‑50ng/mL sufficient for most health outcomes.
How much Vitamin D do you need?
The Institute of Medicine (now Health Canada) recommends 600IU per day for adults up to 70years and 800IU for those older. However, recent meta‑analyses show that maintaining serum 25(OH)D above 30ng/mL often requires 1000‑2000IU daily, especially for people with limited sun.
For high‑risk groups, a short‑term loading phase-10,000IU per day for 4weeks-can safely raise levels, followed by a maintenance dose of 2000-4000IU. Always check with a health professional before starting high‑dose regimens.
Getting Vitamin D from food and sun
Natural food sources are few but potent:
- Fatty fish (salmon, mackerel, sardines): 400-600IU per 100g
- Cod liver oil: roughly 450IU per teaspoon
- Egg yolk: about 40IU each
- Mushrooms exposed to UV light: up to 200IU per 100g
Fortified products-milk, orange juice, plant‑based milks-add another 100-150IU per serving. Sunlight remains the cheapest source: 10‑15minutes of midday exposure to face, arms, and legs twice a week can generate 1000IU, provided skin isn’t covered and the UV index is above 3.
Remember, sunscreen with SPF30 cuts Vitamin D synthesis by about 95%. A brief, uncovered exposure before slathering on sunscreen works best.

Supplementation: Vitamin D3 vsD2
When diet and sun aren’t enough, supplements fill the gap. Two main forms exist:
| Attribute | Vitamin D3 | Vitamin D2 |
|---|---|---|
| Source | Animal‑derived (lanolin, fish oil) | Plant‑derived (ergosterol from fungi) |
| Potency | ~30% more effective at raising serum 25(OH)D | Lower bioavailability |
| Half‑life | ~2weeks | ~1week |
| Typical dose range | 1000-4000IU daily | 2000-8000IU daily (to match D3 effect) |
Because D3 stays in the bloodstream longer and converts more efficiently, most clinicians recommend it for routine supplementation.
Monitoring and preventing hypocalcemia
Even with supplementation, checking labs is wise. A basic panel should include:
- Serum calcium total calcium concentration in the blood
- Serum 25(OH)D
- Parathyroid hormone (PTH) regulatory hormone that rises when calcium is low
- Phosphate
If calcium is low but PTH is high, Vitamin D deficiency is likely. Raising Vitamin D intake usually brings both numbers back into range within 8-12weeks.
Avoiding hypocalcemia also means not over‑correcting. Excessive Vitamin D can push calcium too high, leading to vascular calcifications. Keep daily intake below 4000IU unless supervised.
Putting it all together: a practical checklist
- Assess risk: age>65, limited sun, darker skin, certain meds.
- Order a blood test for serum 25(OH)D and calcium.
- If 25(OH)D<20ng/mL, start 1000-2000IU Vitamin D3 daily.
- Include two servings of fatty fish or fortified foods each week.
- Get 10‑15minutes of midday sun twice weekly, weather permitting.
- Re‑test after 8 weeks; adjust dose to keep 25(OH)D between 30‑50ng/mL.
- Monitor calcium and PTH if you have kidney disease or take thiazide diuretics.
Frequently Asked Questions
Can I get enough Vitamin D from sunlight in Toronto?
During the summer months, short midday exposures three times a week usually suffice. In winter, the sun angle is too low for UV‑B synthesis, so diet or supplements become necessary.
What symptoms signal hypocalcemia?
Common signs include tingling around the mouth and fingertips, muscle cramps, especially in the calves, and in severe cases, cardiac palpitations or seizures.
Is Vitamin D2 ever preferred over D3?
D2 is useful for strict vegans because it’s plant‑derived, but achieving the same blood level typically requires a higher dose. Most clinicians still favor D3 for its stronger effect.
How often should I test my Vitamin D status?
If you’re starting supplementation, check after 8-12 weeks. Once stable, an annual test is enough unless you have a condition that affects absorption.
Can high Vitamin D intake cause health problems?
Excessive Vitamin D can raise calcium too high, leading to kidney stones or soft‑tissue calcification. Staying under 4000IU per day for adults-unless a doctor advises otherwise-avoids this risk.







Comments
Taylor Van Wie
6 October 2025Get your damn vitamin D levels checked, folks-America’s health depends on it!
carlee Lee
7 October 2025Vitamin D helps absorb calcium, so keep sunlight and supplements in balance.
chuck thomas
7 October 2025Ever wonder why low vitamin D spikes hypocalcemia risk? The body needs that sunshine‑derived hormone to coax calcium into the bloodstream. When D is lacking, the gut’s absorption efficiency plummets, leaving you vulnerable. It’s a cascade that can sneak up on anyone, especially older adults.
Gareth Pugh
8 October 2025Think of vitamin D as the VIP usher for calcium at the club of your bones. Without its badge, calcium gets turned away at the door. The chemistry is simple yet elegant, and it’s why we all need a daily dose of sunshine or supplements.
Illiana Durbin
8 October 2025That’s a solid breakdown of the mechanism. I’ve seen patients who thought they were fine until a routine blood test revealed low 25‑OH‑D. Adding a modest 800‑1000 IU of vitamin D daily usually normalizes levels within a few weeks. Pair it with calcium‑rich foods like dairy, leafy greens, and fortified cereals for best results.
Don’t forget to re‑test after three months to make sure the numbers have improved.
Tyler Heafner
9 October 2025Indeed, the interplay between vitamin D and calcium is fundamentally biochemical. It is advisable to monitor serum 25‑OH‑D periodically, especially in at‑risk populations. Supplementation should be calibrated to individual baseline levels. A follow‑up assay after a quarter is prudent.
anshu vijaywergiya
10 October 2025Picture a sunrise spilling gold across the horizon, quietly awakening every cell in your body. That golden glow is the catalyst that unlocks calcium’s hidden potential. When the light fades, the cascade stalls, and the body’s calcium reserves whisper for rescue. So whether you’re a desk‑bound coder or a field‑working farmer, seek that daily glow.
ADam Hargrave
10 October 2025Oh sure, just slap a vitamin D pill on your fridge and call it a day-because that’s how biology works, right? In reality, the mind‑boggling chemistry requires more than a casual suggestion. Sunlight, diet, and maybe a prescription are the real players here.
Michael Daun
11 October 2025lol that sarcasm tho
but yea, vitamins not magic
Rohit Poroli
11 October 2025From a clinical pharmacology standpoint, vitamin D functions as a secosteroid hormone, modulating transcription of calcium‑binding proteins. Deficiency impairs the intestinal calcium channel activity, precipitating hypocalcemic episodes. It’s essential to assess both total serum 25‑OH‑D and ionized calcium for a comprehensive picture. Integrating these markers into routine panels can preempt adverse outcomes.
William Goodwin
12 October 2025💡 Pro tip: A quick 10‑minute walk outside around midday can boost your D levels faster than a pill.
🌞 And don’t forget those fortified plant milks if you’re dairy‑free! 🚀
Isha Bansal
13 October 2025Allow me to point out the egregious grammatical errors that pepper this discussion. Firstly, the phrase “vitamin D helps the gut absorb calcium” should be punctuated with a semicolon when followed by an independent clause. Secondly, “low serum 25(OH)D (65” is a malformed parenthetical; the closing parenthesis is missing. Thirdly, the usage of “limited sun, darker skin, certain meds.” lacks parallel structure; a colon would be more appropriate. Fourthly, “Order a blood test for serum 25(OH)D and calcium.” should be a directive, not a fragmented sentence. Lastly, the concluding bullet point is cut off, rendering the passage incomplete. Please rectify these issues for clarity.
Ken Elelegwu
13 October 2025I appreciate the meticulous attention to detail; it elevates the discourse.
Addressing the grammatical concerns will certainly enhance readability.
Your dedication to precision is commendable.
Gene Nilsson
14 October 2025It is absolutely essential that each individual recognizes the profound impact of vitamin D on calcium metabolism. Neglecting this vital nutrient equates to compromising one's physiological integrity. Consequently, disciplined supplementation, alongside dietary vigilance, becomes a moral imperative. The ramifications of omission can be severe.
Vintage Ireland
14 October 2025Honestly, just get out in the sun when you can and toss a D supplement in your routine. It’s not rocket science.
Anshul Gupta
15 October 2025People love to overcomplicate this, but the answer is simple: take vitamin D or risk low calcium.
Maryanne robinson
15 October 2025When you think about the cascade that begins with a photon of sunlight striking the skin, you realize we’re looking at one of nature’s most elegant systems. The UVB radiation converts 7‑dehydrocholesterol into previtamin D3, which then thermally isomerizes into cholecalciferol. This molecule travels to the liver, where it becomes 25‑hydroxyvitamin D – the primary circulating form we measure in labs. From there, the kidneys hydroxylate it to 1,25‑dihydroxyvitamin D, the active hormone that binds to nuclear receptors in intestinal cells. By engaging these receptors, it up‑regulates the transcription of calbindin and other calcium‑binding proteins, effectively opening the gates for calcium to be absorbed. Without sufficient D, those gates stay shut, and the body siphons calcium from bone, leading to demineralization over time. Studies have shown that even modest increases in serum 25‑OH‑D (from 15 to 30 ng/mL) can improve calcium absorption efficiency by 20‑30 percent. Moreover, elderly populations, who often have reduced skin synthesis capacity, benefit disproportionately from supplementation. Clinical guidelines now recommend at least 800–1,000 IU daily for adults over 65, with higher doses for those with confirmed deficiency. It’s also worth noting that excessive calcium intake without adequate vitamin D can result in soft tissue calcifications, underscoring the need for balance. For anyone tracking their health metrics, regular re‑assessment of both vitamin D and calcium levels every three to six months is prudent. Finally, lifestyle factors such as limited outdoor activity, high latitude living, and the use of sunscreen can all blunt vitamin D synthesis, so dietary sources like fatty fish, fortified foods, and purposeful supplementation become essential. In summary, maintaining optimal vitamin D status is not a luxury; it’s a cornerstone of calcium homeostasis and overall skeletal health.