Medication Safety Checker for Post-Menopausal Women
Medication Safety Assessment
Identify potential risks in your medication regimen based on post-menopausal physiology and Beers Criteria
This tool helps you identify potential medication risks. It is not a substitute for professional medical advice. Always consult your healthcare provider before making any changes to your medications.
Your Medications
Assessment Summary
How to Use This Tool
Step 1: Add all medications you're currently taking
Step 2: Click "Analyze My Medications"
Step 3: Review your personalized safety assessment
Important: This tool is designed to identify potential medication risks based on evidence-based guidelines. It should be used as a conversation starter with your healthcare provider. Always discuss any changes to your medication regimen with your doctor.
Why Medication Safety Changes After Menopause
After menopause, your body doesn’t just stop having periods-it starts processing medications differently. Hormone levels drop, liver function slows, kidney clearance decreases, and body fat increases. These aren’t minor shifts. They change how drugs are absorbed, broken down, and eliminated. A pill that was safe at 45 might become risky at 65. And with most post-menopausal women taking 4 to 5 prescription drugs daily, the chance of dangerous interactions grows fast.
The real danger isn’t one wrong pill. It’s the slow buildup of overlapping risks: a blood thinner plus an NSAID, estrogen therapy with a history of migraines, or antidepressants that worsen dry eyes and urinary issues. The Agency for Healthcare Research and Quality found that 35% of hospitalizations in women over 65 are caused by adverse drug events. That’s not rare. That’s routine.
What Hormone Therapy Can and Can’t Do
Hormone therapy (MHT) is still the most effective treatment for hot flashes and night sweats-but it’s not for everyone. The Endocrine Society and U.S. Preventive Services Task Force agree: estrogen alone (for women without a uterus) is safer than combined estrogen-progestin therapy. But even estrogen carries risks.
Here’s what’s absolutely off-limits: if you’ve had breast cancer, a blood clot, stroke, heart attack, or unexplained vaginal bleeding, you should not take estrogen. Period. Even transdermal patches aren’t safe in these cases.
For others, the timing matters. Starting hormone therapy within 10 years of menopause-or before age 60-may lower heart disease risk. Starting later? The risks rise. A 2018 meta-analysis in Menopause showed transdermal estrogen reduces blood clot risk by 30-50% compared to pills. That’s why patches or gels are now the first choice for women with even mild clotting risks.
And don’t assume “natural” means safe. Bioidentical hormones aren’t FDA-regulated. They’re mixed in compounding pharmacies with no standard testing. The same risks apply-without the safety data.
Non-Hormonal Alternatives That Actually Work
If you’re afraid of hormone therapy, you’re not alone. Nearly 60% of women stop it within a year because of fear-mostly around breast cancer. But there are effective non-hormonal options.
- SSRIs like paroxetine reduce hot flashes by 50-60%. They’re FDA-approved for this use. But they can cause low libido, weight gain, or nausea in 30-40% of users.
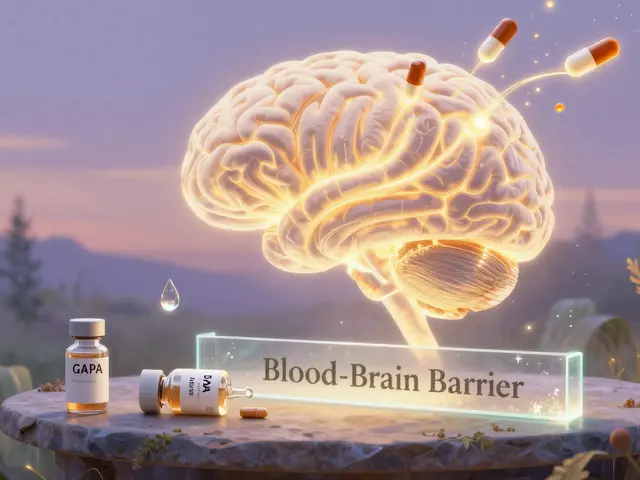
- Gabapentin helps night sweats and sleep. It’s not a hormone, but it can cause dizziness or swelling in older women.
- Clonidine, a blood pressure drug, reduces hot flashes but can cause dry mouth and low blood pressure-risky if you’re already on other heart meds.
- Fezolinetant, a newer drug approved in 2023, blocks brain signals that trigger hot flashes. No estrogen. No blood clots. But it’s expensive and requires liver monitoring.
Many women don’t know these exist. A Reddit survey of 1,245 women in r/menopause (2023) found 63% struggled to find doctors who knew about non-hormonal options. That’s a gap in care-and it’s leaving women suffering unnecessarily.

Polypharmacy: The Silent Killer
“Polypharmacy” sounds like a medical term, but it’s simple: taking five or more medications. And 44% of post-menopausal women do. That’s not because they’re overmedicated-it’s because they have arthritis, high blood pressure, osteoporosis, diabetes, and maybe depression. Each condition gets its own doctor. Each doctor writes a prescription. No one looks at the whole list.
The World Health Organization calls this a global crisis. Why? Because when you take multiple drugs, the chance of a bad interaction skyrockets. Take this real case: a 72-year-old woman on diclofenac (for arthritis), simvastatin (for cholesterol), enalapril (for blood pressure), and atenolol (for heart rate). She developed a bleeding ulcer. Why? Diclofenac and aspirin (which she was also taking) both thin the blood. Her doctor never asked about over-the-counter meds.
The Beers Criteria (2019) lists 30 drugs to avoid in older women, including:
- Long-acting benzodiazepines (like diazepam)-they increase hip fracture risk by 50%
- Anticholinergics (like diphenhydramine)-linked to dementia
- NSAIDs like ibuprofen-raise heart and kidney risks
And here’s the kicker: 28% of women still make medication errors-taking a pill twice, or missing doses. Pill organizers help, but only if they’re used correctly.
Deprescribing: When Stopping Is the Right Choice
Most doctors focus on adding meds. Few focus on removing them. That’s a problem. The WHO found that structured deprescribing reduces medication burden by 1.4 drugs per person-and cuts adverse events by 33%.
Deprescribing isn’t about quitting drugs cold turkey. It’s about slow, smart tapering:
- Benzodiazepines: taper over 8-12 weeks
- Antidepressants: taper over 4-8 weeks
- Statins: consider stopping if you’re over 75 and have no heart disease
- Proton pump inhibitors (PPIs): stop after 4-8 weeks unless you have ulcers or GERD
The START/STOPP criteria help doctors spot what’s missing and what’s harmful. For example, many older women don’t get enough calcium or vitamin D-but they’re on five other pills. A simple supplement could prevent a fracture. But no one checks.
How to Take Control of Your Medications
You don’t need to be a medical expert to stay safe. Here’s what works:
- Keep a living list of every pill, vitamin, herb, and supplement. Include the reason you take it, the dose, and who prescribed it.
- Bring everything to every appointment-the real bottles, not a list. This is called a “brown bag review.”
- Ask your pharmacist for a medication review. Pharmacists are trained to spot interactions. Many offer this for free.
- Ask: “Is this still needed?” after every hospital visit or new diagnosis.
- Use a pill organizer with alarms. JAMA found they reduce errors by 81%.
And don’t be afraid to say: “I don’t want to take this anymore.” Your body changes. Your meds should too.
The Big Picture: It’s Not Just About Pills
Post-menopausal health isn’t about fixing one symptom. It’s about managing multiple conditions without making things worse. Women in this group are more likely to be on multiple drugs, see multiple doctors, and face side effects that are dismissed as “just aging.”
The NIH is investing $25 million into research on non-hormonal menopause treatments. New tools like AI-driven medication reconcilers are cutting errors by 45%. But until those tools reach every clinic, you’re your own best advocate.
There’s no one-size-fits-all plan. But there is a clear path: know your meds, question every new prescription, and never assume something is safe just because your doctor prescribed it. Your body after menopause deserves more than a checklist. It deserves a plan that fits you.
Is hormone therapy safe after menopause?
Hormone therapy can be safe for some women, but only under specific conditions. It’s safest when started within 10 years of menopause or before age 60, using the lowest effective dose. Transdermal estrogen (patches or gels) is preferred over pills because it lowers the risk of blood clots. It’s not safe if you’ve had breast cancer, a blood clot, stroke, heart attack, or unexplained vaginal bleeding. Always discuss your personal risk factors with your doctor.
Can I stop taking my statin after menopause?
Maybe. If you’re over 75 and don’t have heart disease, diabetes, or a history of stroke or heart attack, the benefits of statins become less clear. The Beers Criteria suggests considering deprescribing in older adults without cardiovascular risk. Never stop on your own-talk to your doctor about a slow taper and whether your cholesterol levels still require treatment.
Why do I keep getting medication errors even with a pill organizer?
Pill organizers help, but they’re not foolproof. Common errors happen when you take the same pill twice because you forgot you already took it, or when you miss a dose because the organizer isn’t labeled clearly. Make sure your organizer has clear labels for morning, afternoon, and night. Also, check if any of your meds need to be taken on an empty stomach or with food-some pills shouldn’t be mixed. Keep your updated medication list next to the organizer.
Are herbal supplements safe for post-menopausal women?
Many herbal supplements aren’t tested for safety in older women or with prescription drugs. Black cohosh, red clover, and soy isoflavones are often used for hot flashes, but they can interact with blood thinners, thyroid meds, or breast cancer treatments. Plus, supplements aren’t regulated by the FDA. One study found 25% of herbal products contained hidden prescription drugs. Always tell your doctor what you’re taking-even if you think it’s “natural.”
How often should I have a medication review?
At least once a year. But you should also have a review after any hospital stay, when you start or stop any medication, or if you’re prescribed two or more new drugs at once. Medicare Part D requires annual medication therapy management for people with multiple chronic conditions. Ask your pharmacist or primary care provider to run a full check-don’t wait for a problem to happen.
What to Do Next
Start today. Grab your pill bottles. Write down every medication, including vitamins and herbs. Bring them to your next appointment. Ask your doctor: “Which of these are still necessary?” and “Is there a safer alternative?” Don’t wait for a hospital visit to realize you’re taking too much. Small steps now can prevent big problems later.





Comments
Derron Vanderpoel
19 November 2025i just took my whole pill organizer to the doc today and she looked at it like i'd brought a dead raccoon. like... yeah, i know it's a mess. but i'm 67 and i'm still alive. somehow.
also, i take melatonin for sleep and i didn't think it counted as a 'med' until you said it. now i'm scared.
Andy Feltus
19 November 2025Let me get this straight. We’ve turned menopause into a pharmaceutical buffet where every doctor is a chef throwing in another spice because ‘why not?’ and the patient is the soup.
Meanwhile, the real solution-sleep, movement, less sugar, less stress-isn’t patented. So it’s not monetizable. Hence, we’re all just walking polypharmacy bingo cards.
And yes, I know. I’m the guy who says ‘just walk more.’ But if you’ve got a 72-year-old woman on 8 meds and a PPI for a PPI-induced PPI dependency… maybe we’re not treating the disease. Maybe we’re just treating the side effects of treating the side effects.
Dion Hetemi
20 November 2025This post is basically a 3000-word PSA for people who don’t read labels. Congrats. You’ve written the manual for how to not die from your own pharmacy.
But let’s be real-most women over 65 don’t have time for brown bag reviews. They’re juggling grandkids, caregiving, and Medicare paperwork. And their doctors? They’re in and out in 7 minutes.
So yeah, this is great advice. Too bad it only works if you have a PhD in pharmacology and a personal assistant.
Kara Binning
22 November 2025I AM SO TIRED OF THIS. I WAS ON 6 MEDS WHEN I TURNED 60. I TOOK THEM ALL FOR YEARS. THEN I STARTED READING. I STOPPED 3. I WENT TO A NATURAL DOCTOR. I GOT MY VITAMIN D UP. I STARTED WALKING. I GOT RID OF MY PPI. I’M NOT ON STATINS. I’M NOT ON ANTIDEPRESSANTS. I’M NOT ON BETA BLOCKERS.
MY BLOOD PRESSURE IS BETTER. MY JOINTS DON’T HURT. I SLEEP LIKE A BABY.
AND NOW MY DOCTOR SAYS I’M ‘NONCOMPLIANT.’ NONCOMPLIANT? I’M ALIVE. I’M VIBRANT. I’M NOT A LAB RAT FOR BIG PHARMA.
river weiss
23 November 2025The most important takeaway here is not the list of medications, but the practice of documentation. A living medication list, updated after every visit, is the single most effective tool for preventing adverse events.
Pharmacists are underutilized. They are the last line of defense against polypharmacy. Many offer free medication therapy management under Medicare Part D.
Also, deprescribing is not failure-it is clinical excellence. If a medication no longer aligns with your goals of care, it should be discontinued. Not because you’re ‘giving up,’ but because you’re choosing quality of life over quantity of pills.
Brian Rono
24 November 2025Let’s call this what it is: medicalized menopause. A natural biological transition turned into a disease state requiring 4-5 pills just to keep you from feeling ‘off.’
And the irony? The same doctors who prescribe you gabapentin for hot flashes will tell you to ‘stop taking that herbal nonsense’-while ignoring that the only reason you started the herbs is because they wouldn’t listen to you in the first place.
Also, ‘bioidentical’ isn’t a medical term. It’s a marketing term invented by compounding pharmacies to sell you snake oil with a fancy label. Don’t be fooled.
Michael Salmon
24 November 2025You people are ridiculous. You’re scared of pills, but you’ll take a $40 bottle of ‘menopause tea’ from a guy on Instagram who says it’s ‘ancient Chinese wisdom.’
Here’s the truth: 90% of these ‘natural’ remedies are untested. Some contain estrogen. Some contain thyroid meds. Some contain heavy metals.
Meanwhile, you’re terrified of FDA-approved SSRIs that have been studied in 10,000 women. You’d rather risk liver failure from a ‘clean’ supplement than take a pill that’s been peer-reviewed.
Stop being emotionally irrational. Medicine isn’t a cult. It’s science.
Joe Durham
26 November 2025I think the real issue isn’t the meds-it’s the system. You’ve got one doctor for your heart, one for your bones, one for your mood, one for your gut. Nobody’s talking. Nobody’s coordinating.
I had a friend who was on 11 meds. She didn’t even know why she was on half of them. Her primary care doc finally sat down with her for 45 minutes and cut 5. She cried. Not because she was sad-because she felt like someone finally saw her.
Timothy Reed
27 November 2025One small step: Before your next appointment, write down three questions:
1. Is this medication still serving me?
2. Is there a non-drug alternative I haven’t tried?
3. What would happen if I stopped this?
These aren’t confrontational questions. They’re collaborative ones. Doctors appreciate patients who are informed-not because they’re challenging them, but because they’re partnering with them.
Christopher K
28 November 2025I’m 70, live in Florida, and I’ve been on the same 5 meds for 12 years. My doctor says ‘if it ain’t broke, don’t fix it.’
So I’m just supposed to keep taking them? Even if I feel like a walking pharmacy?
Meanwhile, my neighbor took herself off her statin and now she’s hiking in the Everglades. Coincidence? I think not.
harenee hanapi
28 November 2025You think this is bad? In India, women over 60 are given 12 different pills just to ‘balance hormones.’ No tests. No reviews. Just a box from the pharmacy. And they call it ‘Ayurveda.’
But you? You have access to the Beers Criteria. You have access to pharmacists. You have access to Reddit.
So stop complaining. Get organized. Or don’t. But don’t act like you’re the victim when you’ve got more resources than 90% of the world.
Christopher Robinson
29 November 2025I started a pill organizer with color-coded slots + alarms 📱⏰
Also wrote down every med + reason + prescriber on a sticky note and taped it to my fridge 🧊
Best decision I ever made. My husband said I’m ‘too organized’... but I haven’t missed a dose in 8 months. And my doctor was shocked I knew what everything was for 😅
James Ó Nuanáin
29 November 2025The notion that ‘natural’ equates to ‘safe’ is not only scientifically baseless-it is dangerously misleading. The notion that ‘more pills = better care’ is a relic of 20th-century medicine. We are now in an era of precision geriatrics.
Deprescribing is not abandonment. It is stewardship.
And yes-pharmacists should be central to this process. Their training in pharmacokinetics and drug interactions is unmatched.
It is not a failure of the patient. It is a failure of the system to integrate multidisciplinary care.
Let us not confuse convenience with competence.