How the FDA Stops Unsafe Drugs Before They Reach You
Every year, more than 100 million drug shipments enter the United States. Most come from overseas manufacturers in countries like India, China, and Germany. The FDA doesn’t inspect every single one. But it doesn’t need to. Instead, it uses a smart, risk-based system to catch the bad ones before they hit pharmacy shelves, hospital stockrooms, or your medicine cabinet.
It’s not magic. It’s a mix of technology, data, and strict rules - all built to protect public health. If you’re a pharmacist, a small biotech startup, or just someone who takes medication daily, understanding how this system works matters. Because when it fails, people get sick. When it works, you never even know it was there.
The Five Steps of an FDA Drug Inspection
The FDA doesn’t just show up at ports with clipboards. Every drug shipment goes through five clear stages before it’s cleared or rejected.
- Entry Submission - The importer (or their customs broker) files electronic paperwork through the FDA’s system. This includes the product name, manufacturer, quantity, and where it’s going. Missing or wrong info? The system flags it immediately.
- Entry Review - Over 98% of entries are screened by automated tools. These tools check the company’s history, past violations, country of origin, and product type. If something looks risky - like a shipment from a facility with a history of cGMP violations - it gets bumped to human review.
- Examination and Sampling - About 1 in 7 shipments gets physically checked. That means inspectors open boxes, check labels, verify storage conditions, and take samples for lab testing. Some shipments get a full lab analysis; others just get a visual inspection. The decision depends on risk level, not luck.
- Compliance Review - If the product fails inspection, the FDA checks if it violates U.S. standards. Is it mislabeled? Was it made in an unregistered facility? Does it contain banned ingredients? This step determines whether the shipment is detained or released.
- Final Admissibility Decision - The FDA makes the call: release, destroy, or recondition. In 2022, nearly 14% of physically inspected drug shipments were detained. Of those, over two-thirds were refused entry entirely.
This system isn’t perfect. But it’s designed to catch the biggest threats first - not waste time on low-risk shipments from trusted suppliers.
Who Gets Scrutinized - and Who Gets a Pass
Not all drug importers are treated the same. The FDA has a special program called the Secure Supply Chain Pilot Program (SSCPP). It’s like a trusted traveler program for pharmaceutical companies.
To qualify, a manufacturer must:
- Have zero serious compliance violations in the last three years
- Pass a full audit of their quality control systems
- Designate up to five products for expedited clearance
As of late 2023, only 27 companies made the cut - big names like Johnson & Johnson and Pfizer. For them, shipments clear in under two days instead of 7-10. That’s a game-changer for just-in-time manufacturing.
But for everyone else? The system is slower and more unpredictable. Generic drug makers, especially those sourcing active ingredients from India or China, face detention rates as high as 37% - even if they’re compliant. Why? Because past violations at their facilities or their country’s inspection history raise red flags.
And here’s the catch: the FDA doesn’t have enough staff to inspect more than 1.2% of all drug shipments physically. That means 98.8% rely on paper reviews and risk algorithms. That’s why the 2022 valsartan contamination slipped through - the contaminated API came in under a low-risk flag and wasn’t sampled.

The Big Change: No More 0 Loophole
Until October 2023, small shipments under $800 could slip into the U.S. without FDA review. That was called the “de minimis” exemption. It was meant for gifts and personal items. But criminals exploited it.
Counterfeit pills, unapproved weight-loss drugs, and even fake insulin were being shipped in small packages through USPS and private couriers. The FDA couldn’t track them. The DEA couldn’t stop them. In 2022 alone, an estimated $4.3 billion in fake drugs entered the U.S. this way.
On October 17, 2023, that loophole vanished. Now, every FDA-regulated drug shipment - no matter how small or cheap - must be declared and reviewed.
The impact? More than 350,000 additional entries per year now go through the FDA’s system. Academic labs that import research samples saw costs jump $285-$420 per shipment. Small biotech firms now need full compliance teams just to ship test materials. But the trade-off is clear: fewer fake drugs reaching patients.
Why Some Ports Are Harder Than Others
Not all U.S. ports are created equal when it comes to drug inspections.
At the Port of Los Angeles, only 5.2% of drug shipments get detained. At the Port of Miami? That number jumps to 18.7%. Why?
- Volume - Miami handles more generic drug shipments from Latin America and India.
- Staffing - Some ports have more experienced FDA inspectors.
- History - Ports with past violations get more scrutiny.
Importers who ship regularly learn which ports are friendlier. Some even route shipments through specific ports to avoid delays. But that’s risky. The FDA’s Harmonized Real-Time Alert System shares inspection data across all 330+ ports. If a shipment gets flagged in Miami, it can be held in Seattle - even if it’s a completely different product.
What Gets You Detained - And How to Avoid It
Most detained shipments fail for the same reasons:
- Incorrect product coding - 28% of delays come from wrong HS codes or FDA product categories.
- Missing registration - The facility making the drug must be registered with the FDA. So must the U.S. agent.
- Labeling errors - Missing lot numbers, expiration dates, or required warnings? That’s a violation.
- Unapproved ingredients - Even one unapproved additive can trigger a detention.
And here’s the worst part: if your shipment gets detained once, you might get placed on an Import Alert. That means every future shipment from that company gets automatically held - no review, no exceptions. Getting off an Import Alert can take months.
The fix? Triple-check your paperwork. Use the FDA’s Electronic Entry Interface Repository (EEIR) to validate your submission format. And if you’re new to this, hire a customs broker who specializes in pharmaceuticals - not just any logistics company.
What’s Next for FDA Drug Imports
The FDA isn’t standing still. Its five-year plan includes:
- AI-powered risk scoring - By 2025, the system will use machine learning to predict which shipments are most likely to be violative - improving detection by 22-28%.
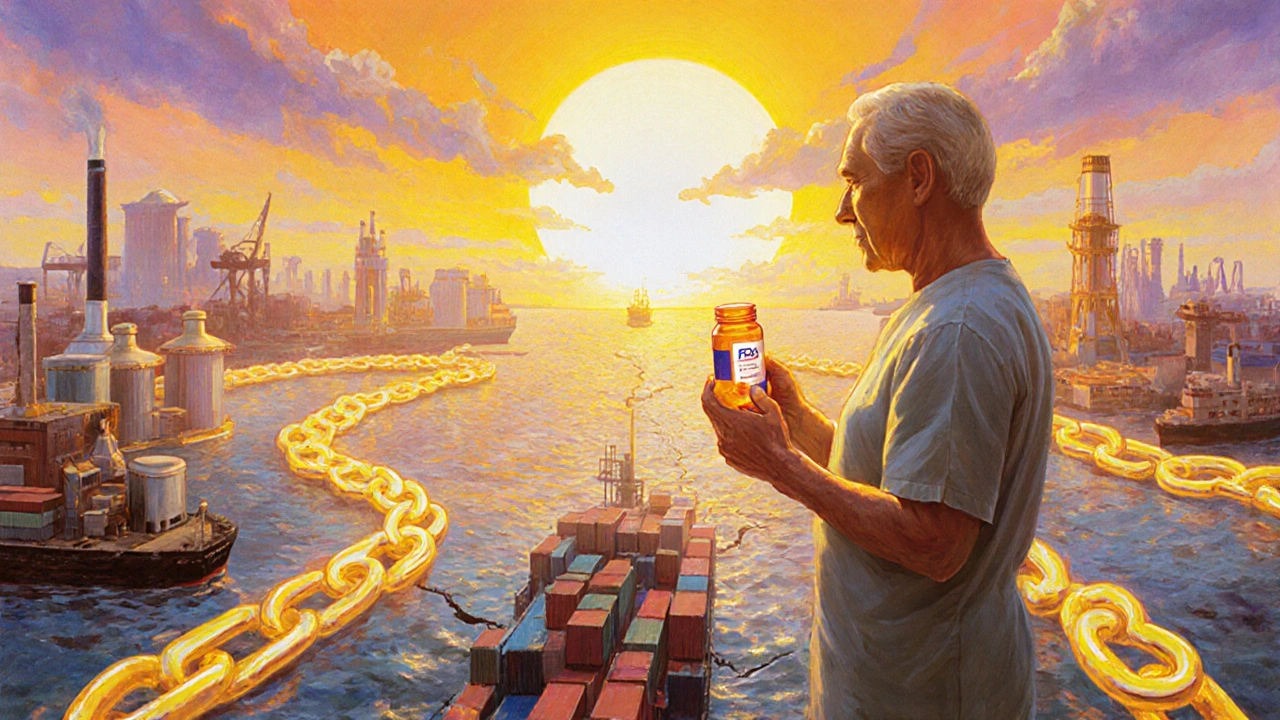
- Blockchain pilots - Starting in early 2024, select companies will test blockchain tracking for API shipments. Think of it like a tamper-proof digital ledger for drug ingredients.
- Expanding SSCPP - The number of approved companies will grow from 27 to 50 by mid-2024. For the first time, contract manufacturers (CMOs) can join - a big win for smaller drug makers who outsource production.
- Global alignment - The FDA is working with the Pharmaceutical Inspection Co-operation Scheme (PIC/S) to recognize inspections from other countries, reducing redundant checks.
But challenges remain. The FDA still doesn’t have enough inspectors. And the rise of online pharmacies selling directly to U.S. consumers - 41% of which operate outside U.S. law - is a growing blind spot.
What This Means for You
If you’re a patient: You can trust that the FDA is actively blocking dangerous drugs. But you should still buy from licensed pharmacies. Avoid websites that sell pills without a prescription.
If you’re a small biotech or generic drug maker: The system is harder than ever. Compliance isn’t optional - it’s your lifeline. Budget for legal help, broker fees, and extra time. Don’t assume your shipment will clear quickly.
If you’re a pharmacist or hospital buyer: Know your suppliers. Ask for their FDA registration number and inspection history. If a generic drug suddenly becomes cheaper or arrives faster than usual - dig deeper.
The FDA’s system isn’t flawless. But it’s the best we have. And it’s getting smarter.
Does the FDA inspect every drug shipment entering the U.S.?
No. The FDA inspects only about 1.2% of drug shipments physically. The rest are reviewed electronically using risk-based algorithms. But since October 2023, every shipment - no matter how small - must be declared and reviewed before entry.
What happens if a drug shipment is detained by the FDA?
The importer gets notified and has a chance to fix the issue - like relabeling, retesting, or providing missing documentation. If the problem can’t be resolved, the shipment is either destroyed or returned to the sender. In 2022, 67.8% of detained shipments were refused entry.
Can I import drugs for personal use?
It’s technically illegal to import prescription drugs for personal use unless they’re FDA-approved. The FDA sometimes allows small quantities (up to a 3-month supply) for serious conditions if no U.S. alternative exists - but this is rare and done at the agency’s discretion. Never buy drugs from foreign online pharmacies.
What’s the difference between FDA and CBP inspections?
CBP handles customs duties, tariffs, and general import rules. The FDA checks for safety, labeling, and compliance with pharmaceutical regulations. Both agencies inspect shipments, but they focus on different things. CBP sees the package; the FDA checks what’s inside.
Why do some generic drugs get detained more than brand-name drugs?
Generic manufacturers often source active ingredients from countries with weaker inspection systems. The FDA has a longer history of violations at certain facilities in India and China. Even if a specific shipment is clean, the company’s past record can trigger automatic holds. Brand-name companies usually have better compliance records and often qualify for expedited programs like SSCPP.
How can I check if a drug manufacturer is FDA-registered?
Go to the FDA’s Drug Establishment Registration database (https://www.accessdata.fda.gov/scripts/drugregistration/). You can search by company name, facility location, or product. If it’s not listed, the product isn’t legally allowed to be sold in the U.S.
What to Do Next
If you’re importing drugs into the U.S., start with the FDA’s Electronic Entry Interface Repository (EEIR). It’s free, updated biweekly, and tells you exactly what forms to file. Don’t guess. Don’t rely on your customs broker’s old templates.
Join an FDA webinar. They’re free and cover everything from labeling rules to how to respond to a detention notice.
And if you’re a patient - stick to licensed pharmacies. The FDA’s system catches most bad drugs. But it’s not a substitute for your own caution.


Comments
King Over
19 November 2025So they're just trusting algorithms to catch fake insulin now? Feels like playing Russian roulette with my diabetes meds
Johannah Lavin
20 November 2025I just found out my grandma's blood pressure med came from a facility that got flagged 3 times last year 😭 The FDA's system is terrifying but also... kinda comforting? 🤔❤️
Ravinder Singh
22 November 2025As someone from India who works in pharma, this hits different. We're not the villains here - it's the systemic bias in the risk models. Our labs meet WHO-GMP standards but still get flagged because of geography, not quality. The SSCPP should be expanded to include CMOs from emerging markets too. It's not about trust - it's about data equity.
Russ Bergeman
22 November 2025Wait... so you're telling me that a $500 shipment of vitamins from a Chinese warehouse is now subject to the same scrutiny as Pfizer's insulin? That's absurd. The FDA is wasting taxpayer money on trivial stuff while real threats slip through. This is bureaucratic overreach at its finest!!!
Dana Oralkhan
24 November 2025I work in hospital pharmacy and I can tell you - the Import Alerts are brutal. One mistake and your entire supply chain gets locked up. We had a generic antiviral get detained for a missing lot number. Took six weeks to resolve. Patients went without. We need more grace periods, not more red tape.
Jeremy Samuel
24 November 2025yeh but like... who even checks this stuff? the FDA has like 200 inspectors for 100 million shipments? sounds like a meme
Destiny Annamaria
25 November 2025OMG I just realized my online order of probiotics from a ‘wellness’ site last month probably didn’t even get reviewed before. I’m so glad that loophole is closed!! 🙌 I don’t want some random guy in a basement selling me fake Adderall. #FDAforthewin
Ron and Gill Day
27 November 2025This is a joke. The FDA is a bloated, outdated bureaucracy that's more interested in control than safety. They detain shipments from India because of historical bias, not current data. They're protecting big pharma monopolies, not patients. And you call this 'smart'? It's just corporate favoritism dressed up as science.
Alyssa Torres
28 November 2025The blockchain pilot? That’s huge. Imagine being able to trace every single molecule of an API from factory to pharmacy. It’s not just about safety-it’s about accountability. And if we can do it for diamonds and coffee, why not life-saving meds? This could be the future of global health equity.
Summer Joy
28 November 2025I'm just waiting for the first viral tweet about someone dying because their insulin was detained for 3 weeks while the FDA 'reviewed' it. This system is a disaster waiting to happen. 😭💀
Aruna Urban Planner
30 November 2025The structural asymmetry in inspection protocols reflects deeper global inequities in regulatory capacity. The FDA's reliance on historical violation data creates path dependency that penalizes emerging economies despite improvements in local GMP standards. A dynamic, real-time risk model calibrated on outcome metrics-not legacy flags-would be more scientifically valid.
Nicole Ziegler
2 December 2025I just checked my last prescription bottle - the lot number matched the FDA database. Feels good to know someone’s watching 👀💊