Antibiotic Selection Tool
Select Your Clinical Scenario
Your Antibiotic Recommendations
When your doctor prescribes a broad‑spectrum antibiotic, you often wonder if there’s a safer, cheaper, or more effective option. Augmentin comparison is a common query, especially for patients who have experienced side effects or who need a targeted treatment. This guide walks through what Augmentin is, why it’s used, and how it stacks up against a handful of widely‑prescribed alternatives.
Key Takeaways
- Augmentin combines amoxicillin with clavulanate to tackle beta‑lactamase‑producing bacteria.
- Common alternatives include amoxicillin alone, cefalexin, azithromycin, doxycycline, clindamycin, and penicillinV.
- Choosing the right drug depends on infection type, resistance patterns, patient allergies, side‑effect profile, and cost.
- For mild ear, sinus, or skin infections, amoxicillin without clavulanate often works just as well.
- Severe or resistant infections may still require Augmentin or a different class such as a cephalosporin.
What Is Augmentin?
Augmentin is a fixed‑dose combination of the penicillin‑type antibiotic amoxicillin and the beta‑lactamase inhibitor clavulanate potassium. It was first launched in 1984 and quickly became a go‑to for mixed‑flora infections because the clavulanate shields amoxicillin from bacterial enzymes that would otherwise break it down.
How Augmentin Works
Amoxicillin interferes with the bacterial cell wall synthesis by binding to penicillin‑binding proteins. Some bacteria produce beta‑lactamase enzymes that destroy the penicillin ring, rendering amoxicillin ineffective. Clavulanate, although a weak antibiotic on its own, binds to those enzymes and disables them, extending amoxicillin’s reach to resistant strains.
Typical Uses for Augmentin
Doctors prescribe Augmentin for a range of infections where beta‑lactamase‑producing organisms are common, such as:
- Acute otitis media (middle‑ear infection)
- Sinusitis, especially when symptoms persist beyond 10 days
- Community‑acquired pneumonia with mixed bacterial flora
- Skin and soft‑tissue infections like cellulitis
- Urinary tract infections caused by Escherichia coli that produce beta‑lactamase
The standard adult dose is 500mg/125mg taken every 8hours, though higher doses (875mg/125mg) are used for more severe infections.
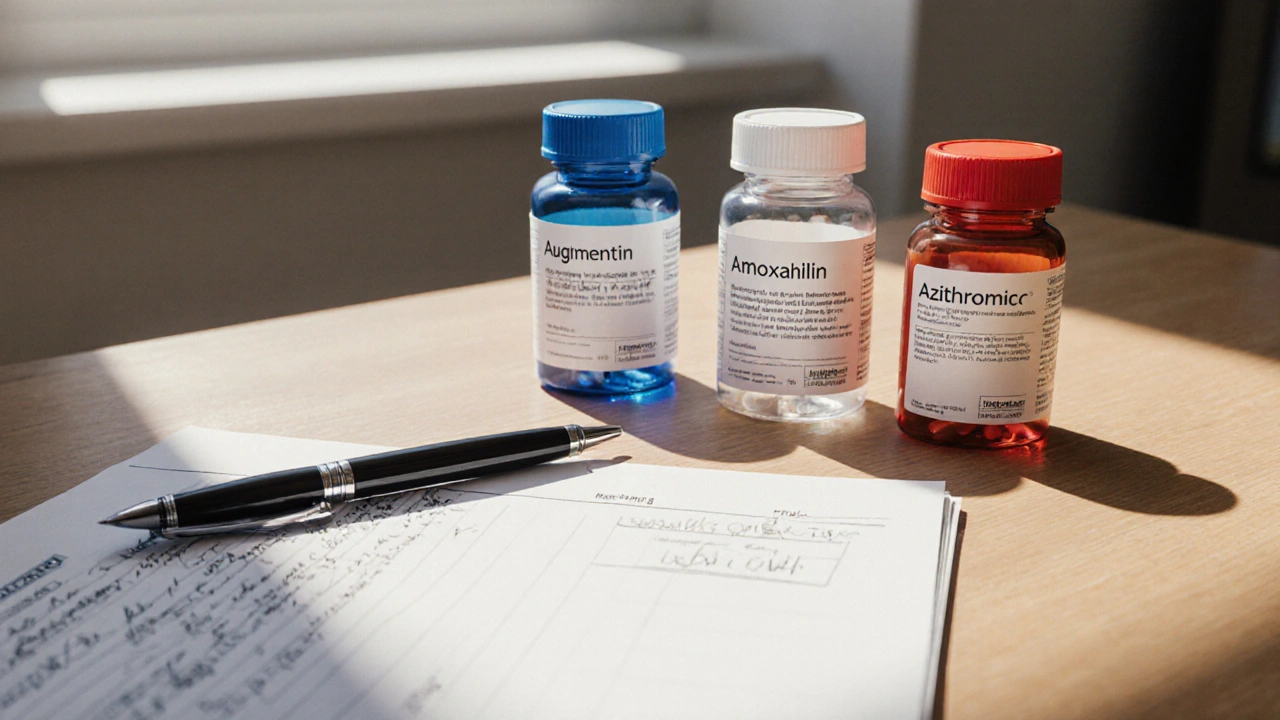
Common Alternatives
Not every infection needs the extra punch of clavulanate. Below are the most frequently considered substitutes.
Amoxicillin is a broad‑spectrum penicillin that targets many of the same bacteria as Augmentin but lacks beta‑lactamase protection. It’s often the first‑line choice for uncomplicated ear and sinus infections.
Cefalexin belongs to the first‑generation cephalosporin class. It resists many beta‑lactamases and is useful for skin, bone, and urinary infections when patients are allergic to penicillins.
Azithromycin is a macrolide that concentrates in tissues and has a long half‑life, allowing once‑daily dosing. It’s popular for atypical pneumonia and certain sexually transmitted infections.
Doxycycline is a tetracycline derivative effective against a broad range of bacteria, including some resistant strains. It’s often used for acne, Lyme disease, and respiratory infections.
Clindamycin is a lincosamide that penetrates bone and abscesses well, making it a choice for serious skin or dental infections, especially in patients allergic to penicillins.
PenicillinV is an oral penicillin with a narrower spectrum than amoxicillin. It’s traditionally used for streptococcal pharyngitis and mild skin infections.
Side‑Effect Profiles
Every antibiotic carries risks. Understanding them helps you weigh benefits against drawbacks.
- Augmentin: Diarrhea (up to 10% of patients), nausea, rash, and rare hepatotoxicity due to clavulanate.
- Amoxicillin: Similar GI upset but less diarrhea; allergic reactions are the most common serious issue.
- Cefalexin: Generally well‑tolerated; may cause mild GI upset and occasional rash.
- Azithromycin: Fewer GI issues, but can cause QT‑prolongation in patients with cardiac risk factors.
- Doxycycline: Photosensitivity and esophageal irritation; avoids in pregnancy.
- Clindamycin: High risk of Clostridioides difficile infection.
- PenicillinV: Classic penicillin allergy symptoms; low GI disturbance.
Antibiotic Comparison Chart
| Drug | Spectrum | Typical Dose (Adult) | Primary Indications | Resistance Concerns | Notable Side Effects |
|---|---|---|---|---|---|
| Augmentin (Amoxicillin/Clavulanate) | Broad - covers many beta‑lactamase‑producing bacteria | 500mg/125mg q8h | Sinusitis, otitis media, pneumonia, skin infections | Increasing beta‑lactamase variants; some ESBL producers | Diarrhea, nausea, liver enzyme elevation |
| Amoxicillin | Broad, but no beta‑lactamase protection | 500mg q8h | Ear, throat, uncomplicated urinary infections | Beta‑lactamase‑producing H. influenzae, M. catarrhalis | Allergic rash, mild GI upset |
| Cefalexin | Moderate - good against gram‑positive and some gram‑negative | 500mg q6h | Skin, bone, urinary tract infections | Penicillin‑binding protein mutations in MRSA | Diarrhea, rash, rare liver issues |
| Azithromycin | Moderate - excellent against atypicals | 500mg daily x3 days | Community‑acquired pneumonia, chlamydia | Macrolide‑resistant S. pneumoniae | QT prolongation, mild GI upset |
| Doxycycline | Broad - includes many resistant organisms | 100mg bid | Lyme disease, acne, respiratory infections | Tetracycline‑resistant Streptococcus | Photosensitivity, esophageal irritation |
| Clindamycin | Broad - strong against anaerobes | 300mg q6h | Severe skin, dental, bone infections | Inducible macrolide‑lincosamide resistance (MLSB) | C.difficile colitis, metallic taste |
| PenicillinV | Narrow - primarily streptococci | 500mg q6h | Strep throat, mild skin infections | Beta‑lactamase‑producing organisms | Allergic reactions, mild GI upset |
Decision‑Making Checklist
Before you or your clinician settle on a prescription, walk through these questions:
- Is the suspected pathogen known to produce beta‑lactamase? If yes, Augmentin or a beta‑lactamase‑stable drug (e.g., cefalexin) is preferable.
- Does the patient have a documented penicillin allergy? If severe (anaphylaxis), avoid Augmentin, amoxicillin, and penicillinV; consider azithromycin or clindamycin.
- Are there cost constraints? Generic amoxicillin and penicillinV are typically cheaper than Augmentin or newer macrolides.
- Is there a high risk for C.difficile infection? Minimize clindamycin and broad‑spectrum penicillins with clavulanate.
- What is the infection site? Tissue penetration matters-clindamycin excels in bone, doxycycline in intracellular pathogens.
Cost and Accessibility in 2025
Canadian pricing data (2024‑2025) shows a typical 14‑day course of generic Augmentin costs about CAD12-15, while generic amoxicillin drops to CAD4-6. Cefalexin sits at CAD8, azithromycin at CAD10, and doxycycline around CAD7. Insurance formularies often prefer the cheaper penicillins unless a beta‑lactamase issue is documented.
Real‑World Scenarios
Scenario1 - Persistent Sinusitis: A 35‑year‑old with 12‑day sinus pain tested positive for H. influenzae producing beta‑lactamase. Augmentin resolved symptoms in 5days, whereas amoxicillin alone failed.
Scenario2 - Simple Strep Throat: A teenager with a rapid strep test received penicillinV. Symptoms cleared in 3days, no need for broader coverage, and cost was minimal.
Scenario3 - Skin Infection in a Penicillin‑Allergic Patient: A diabetic patient with cellulitis and a known anaphylactic reaction to penicillins was switched to clindamycin. The infection improved, but the patient later developed mild C.difficile diarrhea, prompting a switch to doxycycline.
When to Stick with Augmentin
Despite many alternatives, Augmentin remains the best choice for mixed infections where beta‑lactamase‑producing bacteria are likely and where a single oral agent simplifies therapy. It’s also the go‑to for pediatric patients with otitis media, provided there’s no penicillin allergy.
Frequently Asked Questions
Can I take Augmentin if I’m allergic to penicillin?
No. Augmentin contains amoxicillin, which is a penicillin derivative. A true penicillin allergy (especially anaphylaxis) means you should avoid Augmentin and consider alternatives like azithromycin or clindamycin, after discussing with your healthcare provider.
Why does Augmentin cause more diarrhea than amoxicillin alone?
Clavulanate disrupts gut flora more aggressively, creating an environment where opportunistic bacteria proliferate. This leads to a higher incidence of antibiotic‑associated diarrhea.
Is a 5‑day course of Augmentin as effective as a 10‑day course?
For most uncomplicated infections, a 5‑day course (especially the higher‑dose formulation) provides comparable cure rates and reduces side‑effect risk. However, deep‑tissue infections may still need longer therapy.
How do I know if my infection is caused by a beta‑lactamase‑producing bug?
Lab cultures and susceptibility testing are the definitive way. In practice, clinicians often rely on typical patterns-e.g., recurrent otitis media in children or chronic sinusitis suggests beta‑lactamase activity, prompting Augmentin use.
Are there any food or drug interactions with Augmentin?
Take Augmentin with food to improve absorption and reduce stomach upset. Avoid concurrent use of allopurinol without medical advice, as it can increase rash risk. Alcohol isn’t contraindicated, but excessive drinking may worsen GI side effects.
Next Steps
If you’re currently on Augmentin and concerned about side effects, talk to your pharmacist about possibly switching to amoxicillin or another narrower agent. If you have a pending prescription for a different infection, use the decision‑making checklist above to discuss the best option with your clinician.
Remember, antibiotics are powerful tools-using the right one at the right dose minimizes resistance and keeps you healthier in the long run.



Comments
Northern Lass
13 October 2025Allow me to illuminate a perspective scarcely entertained in mainstream discourse: Augmentin, whilst celebrated for its beta‑lactamase inhibition, may in fact be an overengineered relic of a bygone era. Infections such as uncomplicated otitis media frequently resolve with amoxicillin alone, rendering the clavulanate component superfluous. Moreover, the proclivity of clavulanate to perturb the gut microbiota cannot be dismissed as a trivial inconvenience. The prudent clinician, therefore, ought to reserve this broad‑spectrum duo for truly resistant pathogens, lest we perpetuate the tyranny of unnecessary broad‑spectrum exposure. One might argue that cost considerations and stewardship imperatives converge upon a singular, elegant solution: a judicious, targeted monotherapy.
Johanna Sinisalo
18 October 2025Great job laying out the key differences, everyone! Remember, when you’re deciding between Augmentin and a narrower agent, think of the patient’s specific context-allergy status, infection severity, and budget. If the infection is mild and the organism isn’t known to produce beta‑lactamase, amoxicillin can save both money and side‑effects. For higher‑risk patients, especially those with a history of treatment failure, Augmentin remains a reliable fallback. Keep using the decision‑making checklist; it’s a solid tool for clinicians and patients alike.
OKORIE JOSEPH
22 October 2025Stop acting like Augmentin is a miracle drug it isn’t it just adds extra side effects and costs more
Lucy Pittendreigh
27 October 2025It is ethically indefensible to prescribe Augmentin indiscriminately when a cheaper, narrower drug would do the job; such wastefulness fuels antimicrobial resistance and burdens the healthcare system. We must hold ourselves to a higher standard of stewardship, prioritising patient safety over pharmaceutical profit. When clinicians default to the broad‑spectrum option without justification, they betray their oath to do no harm. Let us champion evidence‑based prescribing and reject the gratuitous use of unnecessary clavulanate. The moral imperative is clear: prescribe the right drug, at the right dose, for the right duration.
surender kumar
1 November 2025Ah, the saga of Augmentin versus its humble cousins-truly the opera of modern medicine! Picture this: a lone amoxicillin marching bravely into the middle ear, only to be ambushed by a sneaky beta‑lactamase villain. Enter clavulanate, the dramatic sidekick, swooping in with a flourish of inhibition, saving the day… or perhaps merely adding a subplot of diarrhea and liver woes. Meanwhile, the sly cefalexin tiptoes behind the curtains, whispering “I’m cheaper, I’m effective.” And let us not forget azithromycin, that suave loner who never stays long enough to cause trouble. In the end, the audience-your doctor-must choose the leading role, lest the curtain fall on patient health. So, dear reader, wield this knowledge like a seasoned director, and may your prescriptions always earn a standing ovation.
JOJO Yang
5 November 2025Honestly the whole Augmentin hype is overrated. Sure it covers beta‑lactamase producers but you’re also inviting a whole host of GI issues like diarrhea and nausea-totally not what you want when you’re feeling sick. If you can get away with plain amoxicillin you probaly should, saves cash and side‑effects. The pharma giants love pushin the combo drug ’cause it’s more profitablе and they can charge higher prices. So next time you’re at the pharmacy ask if you really need the extra “clavulanate” drama.
Faith Leach
10 November 2025👊🏼 Wake up, folks! The big pharma cartel pushes Augmentin like it’s the only answer while tiny antibiotic manufacturers get buried under their greed. They claim it’s “broad‑spectrum” but really it’s a cash‑cow feeding the system’s endless profit machine. If you’re in a country that cares about real health, demand cheaper, effective alternatives-don’t let the pharma overlords dictate your prescription. Remember, every unnecessary dose of clavulanate is a win for their bottom line and a loss for our gut flora. 💥 Stay vigilant, stay healthy.
Kate Babasa
15 November 2025In the context of antimicrobial stewardship, the pharmacodynamic profile of Augmentin-comprising amoxicillin (a β‑lactam) synergistically combined with clavulanate potassium (a β‑lactamase inhibitor)-exhibits a broadened antibacterial spectrum, particularly against β‑lactamase‑producing pathogens; however, this expanded coverage is accompanied by an elevated incidence of gastrointestinal adverse events, notably antibiotic‑associated diarrhea. Conversely, monotherapy with amoxicillin alone maintains a favorable safety profile while remaining efficacious against non‑β‑lactamase‑producing organisms, thereby aligning with principles of targeted therapy and cost‑effectiveness. Clinicians should therefore calibrate antibiotic selection based on pathogen susceptibility data, patient allergy history, and pharmacoeconomic considerations, ensuring optimal therapeutic outcomes while mitigating collateral damage to the microbiome. Moreover, the inclusion of cefalexin or doxycycline as viable alternatives may further enhance regimen individualisation, especially in settings with heightened C. difficile risk.
king singh
19 November 2025Thanks for the thorough comparison. It’s useful to see the side‑effect trade‑offs laid out clearly. I’ll keep this in mind when discussing options with patients.
Adam Martin
24 November 2025When we dive into the nitty‑gritty of antibiotic selection, the first thing that should hit the clinician’s mind is the underlying microbiology of the infection in question. Augmentin, with its amoxicillin‑clavulanate duo, was originally engineered to knock out β‑lactamase producers that render plain amoxicillin ineffective, and that purpose still holds true in many real‑world scenarios. That said, the addition of clavulanate is not without cost-both literally in terms of price and biologically in terms of gastrointestinal tolerability, where patients often report diarrhea, nausea, and occasional liver enzyme elevations. For uncomplicated otitis media or sinusitis, a substantial body of evidence now supports the use of amoxicillin alone, which is cheaper, better tolerated, and still achieves high cure rates when β‑lactamases are not a dominant factor. In contrast, when you have risk factors for resistant organisms-such as recent antibiotic exposure, daycare attendance in children, or a history of treatment failure-the wider spectrum of Augmentin can be a lifesaver. Now, let’s not ignore the alternative classes: first‑generation cephalosporins like cefalexin offer reliable gram‑positive coverage with a lower propensity for C. difficile infection, making them attractive for skin and urinary tract infections especially in patients with prior C. difficile episodes. Macrolides such as azithromycin provide convenient once‑daily dosing and excellent intracellular penetration, which is handy for atypical pneumonia, but the rise of macrolide‑resistant Streptococcus pneumoniae limits their utility in many regions. Tetracyclines like doxycycline are broad‑spectrum workhorses that also have anti‑inflammatory properties, yet they are contraindicated in pregnancy and can cause photosensitivity, so they’re not a universal solution. Clindamycin, meanwhile, shines in deep‑tissue infections because of its excellent bone penetration, but its notorious association with C. difficile colitis forces clinicians to reserve it for cases where anaerobic coverage is truly needed. The decision‑making checklist in the original post does a good job of flagging these nuances-particularly the allergy considerations, where a severe penicillin allergy automatically eliminates Augmentin, amoxicillin, and penicillin V from the equation, pushing us toward azithromycin or clindamycin. Cost is another decisive factor; a generic course of Augmentin can easily double the out‑of‑pocket expense compared with amoxicillin, which matters for patients without comprehensive insurance coverage. In practice, I often start with the narrowest effective agent, monitor the clinical response, and reserve broader agents like Augmentin for documented failures or when culture data point to β‑lactamase producers. This “step‑down” approach aligns with antimicrobial stewardship goals and helps preserve the utility of our antibiotic arsenal for the future. Ultimately, the art of prescribing lies in balancing efficacy, safety, cost, and resistance pressures-all of which are well captured in the comprehensive comparison provided. By staying vigilant and evidence‑based, we can ensure patients receive the most appropriate therapy while safeguarding public health.
Ryan Torres
28 November 2025💊🚨 Big pharma wants you on Augmentin because it’s a profit machine – more pills, more patent extensions, more money in their vaults. They disguise it as “broad‑spectrum” while quietly loading your gut with extra clavulanate that triggers diarrhea and even liver stress. If you’re not a pawn in their scheme, ask for a simple penicillin or amoxicillin – it works and they can’t charge you as much. 🕵️♂️ Stay sharp, read the fine print on the prescription, and protect your microbiome from unnecessary assault.
shashi Shekhar
3 December 2025yeah yeah another “comprehensive comparison” but really it’s just a fancy way of saying “pick a cheap pill and stop whining”. you’ll see most doctors just default to Augmentin because it’s the safe bet on paper, but in reality, amoxicillin does the job for most simple infections. if you’re allergic to penicillins, sure, try azithro or doxy but don’t expect miracles – antibiotics aren’t magic.
Marcia Bailey
8 December 2025Excellent summary! 😊 It really helps to see the pros and cons laid out side by side. For anyone feeling overwhelmed, start with the checklist and talk to your pharmacist about cost‑effective options. Remember, the best antibiotic is the one that treats the infection without causing unnecessary side effects. Keep sharing these helpful resources! 👍
Hannah Tran
12 December 2025Let’s cut to the chase: the pharmacokinetic/pharmacodynamic (PK/PD) parameters of Augmentin make it a robust option for polymicrobial infections, but the attendant increase in adverse event (AE) rate, especially Clostridioides difficile‑associated diarrhea, cannot be dismissed as a minor trade‑off. In resource‑constrained settings, the incremental cost‑effectiveness ratio (ICER) often favours amoxicillin or a first‑generation cephalosporin, provided susceptibility patterns support their use. Clinicians should therefore leverage antibiogram data, patient comorbidities, and allergy profiles to tailor therapy rather than reflexively reaching for the broad‑spectrum combo. This evidence‑based, patient‑centered approach mitigates antimicrobial resistance (AMR) pressures while preserving clinical outcomes.
Crystle Imrie
17 December 2025Augmentin is overkill for most simple infections.