Idiosyncratic Drug Reaction Symptom Checker
This tool helps you recognize symptoms that might indicate a rare drug reaction. Remember: It is not a medical diagnosis.
The article explains that idiosyncratic reactions typically appear 1-8 weeks after starting a medication. Symptoms may include fever, rash, yellowing skin, dark urine, or fatigue.
Your Symptoms
Your Medication
Most people know that medications can cause side effects-headaches, nausea, drowsiness. But what if a drug you’ve taken safely for weeks suddenly makes you seriously ill? No one saw it coming. No dose increase. No known interaction. Just a rash, fever, or jaundice that doesn’t make sense. That’s an idiosyncratic drug reaction-a rare, unpredictable, and sometimes deadly response that catches even doctors off guard.
What Makes a Drug Reaction Idiosyncratic?
Not all side effects are the same. About 80 to 85% of adverse reactions are predictable. These are called type A reactions. They happen because the drug does more of what it’s supposed to do. Take too much blood pressure medicine? Your blood pressure drops too low. Take too much acetaminophen? Your liver gets overwhelmed. These are dose-dependent, common, and often avoidable. Idiosyncratic drug reactions (IDRs), or type B reactions, are the opposite. They’re rare-happening in maybe 1 out of every 10,000 to 100,000 people. They don’t follow the rules. You can take the right dose, at the right time, and still end up in the hospital. The reaction isn’t caused by the drug’s intended action. It’s caused by your body’s unexpected response to it. These reactions usually show up after a delay. Most patients don’t get sick until 1 to 8 weeks after starting the drug. That’s why they’re so easy to miss. A patient might think their fever and fatigue are from a cold or the flu. A rash? Maybe it’s allergies. It takes time, and sometimes a lot of testing, to connect the dots back to the medication.The Most Common and Dangerous Types
Not all IDRs look the same. Some affect the skin. Others attack the liver. A few can shut down multiple organs. The most frequent serious IDR is idiosyncratic drug-induced liver injury (IDILI). It accounts for nearly half of all severe drug-related liver damage. It can show up as hepatitis-fatigue, yellow skin, dark urine-or as bile flow blockage, causing itching and pale stools. In about 60% of cases, the liver cells themselves are damaged. In 30%, the bile ducts are affected. A small number have mixed patterns. About 13% of all acute liver failure cases in the U.S. come from IDILI, according to the Hamner-UNC Institute for Drug Safety Sciences. Another group of dangerous IDRs involves the skin and immune system. These are called severe cutaneous adverse reactions (SCARs). They include:- Stevens-Johnson syndrome (SJS): painful blisters and peeling skin, usually starting on the face and chest.
- Toxic epidermal necrolysis (TEN): a more extreme version where large sheets of skin detach-life-threatening.
- DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms): fever, rash, swollen lymph nodes, and organ inflammation, often involving the liver or kidneys.
Why Do Only Some People Get Them?
This is the big mystery. Why does one person react badly to a drug while millions take it without issue? The leading theory is the hapten hypothesis. Some drugs break down in the body into reactive chemicals. These chemicals stick to your own proteins like sticky tape. Your immune system sees these altered proteins as foreign invaders-like a virus-and attacks. This immune response causes the damage. Genetics play a huge role. Certain versions of immune system genes make people more likely to react. The most well-known example is HLA-B*57:01. People with this gene variant have a 50% chance of developing a severe allergic reaction to the HIV drug abacavir. Testing for this gene before prescribing abacavir has nearly eliminated this reaction in clinical practice. Another example is HLA-B*15:02. Carriers of this gene, common in Southeast Asia, are at high risk for SJS or TEN when taking carbamazepine (used for seizures and bipolar disorder). Many countries now require genetic testing before prescribing this drug to people of Asian descent. But here’s the problem: for over 90% of drugs linked to IDRs, we don’t have a genetic test. We can’t predict who’s at risk. That’s why these reactions stay unpredictable.
How Doctors Diagnose Them
Diagnosing an IDR isn’t like checking a blood sugar level. There’s no single test. It’s detective work. Doctors look for three key signs:- Timing: Did symptoms start 1 to 8 weeks after starting the drug?
- Severity: Is the reaction way worse than you’d expect from the dose?
- No other cause: Could it be an infection, autoimmune disease, or another medication?
What Happens After Diagnosis
The first and most important step: stop the drug. Immediately. Treatment depends on the reaction. For mild rashes, antihistamines and topical steroids may be enough. For DRESS or SJS/TEN, hospitalization is often needed. High-dose steroids, intravenous immunoglobulins, or even plasma exchange might be used. Supportive care-fluids, wound care, pain control-is critical. Some patients recover fully. Others don’t. Liver damage can become chronic. Skin scarring from TEN can be permanent. DRESS can lead to long-term thyroid or kidney problems. And the emotional toll? Many patients report being dismissed by doctors at first. “I thought I was going to die,” said one patient on the DRESS Syndrome Foundation forum. “No one believed me until my skin started peeling.”Why This Matters to the Pharmaceutical Industry
IDRs are one of the biggest reasons drugs get pulled off the market. Between 1950 and 2023, 38 drugs were withdrawn in the U.S. mainly because of idiosyncratic toxicity. Troglitazone (for diabetes) was pulled in 2000 after causing fatal liver damage. Bromfenac (a painkiller) was pulled in 1998 after dozens of liver failures. These withdrawals cost the industry billions. The Tufts Center estimates IDR-related failures cost $12.4 billion a year. That includes failed clinical trials, post-market lawsuits, and recalls. To fight this, drug companies now screen for “reactive metabolites” in early development. If a drug breaks down into something too chemically aggressive, it’s often scrapped before it even reaches patients. In 2005, only 35% of companies did this. By 2023, 92% did. Regulators like the FDA and EMA now require detailed metabolite studies. New guidelines, like the 2023 ICH M17, push companies to test for immune-triggering potential early.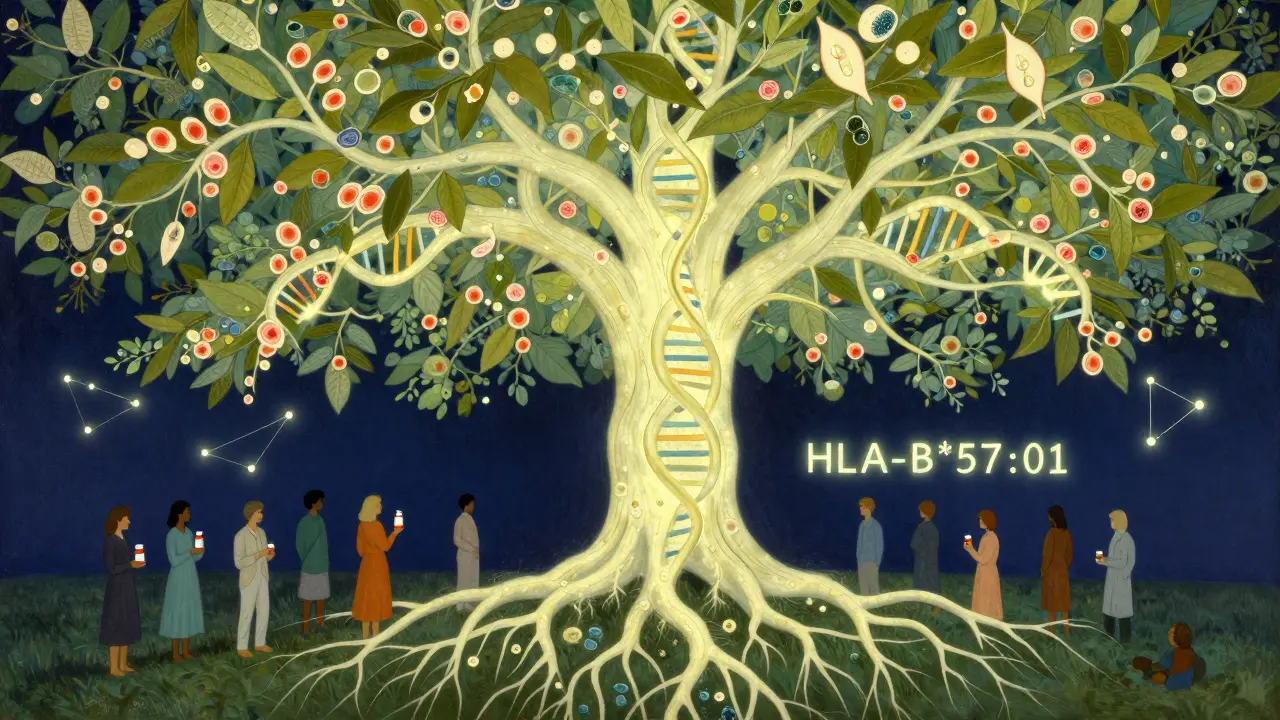
What’s Changing Right Now
The field is finally making progress. In 2023, the FDA approved the first predictive test for pazopanib, a cancer drug that can cause liver injury. The test identifies patients at higher risk based on genetic and liver enzyme markers. Sensitivity: 82%. Specificity: 79%. It’s not perfect, but it’s a breakthrough. Researchers have also found 17 new gene-drug links since 2022. One of them, HLA-A*31:01, predicts phenytoin-induced SJS/TEN. That’s another drug that can now be used more safely in at-risk populations. The NIH is investing $47.5 million in the Drug-Induced Injury Network to study how these reactions start at the cellular level. The European Union’s ADRomics project aims to combine genetic, immune, and metabolic data to build predictive models by 2027. AI tools are being trained on millions of patient records from the FDA’s Sentinel Initiative. These systems look for hidden patterns-like which patients, with which genes, taking which drugs, developed liver injury after 37 days.What You Can Do
If you’re taking a new medication:- Know the warning signs: unexplained fever, rash, yellow eyes, dark urine, severe fatigue, swollen lymph nodes.
- Don’t ignore symptoms that appear weeks after starting a drug.
- Keep a list of all your medications and share it with every doctor.
- If you’ve had a bad reaction to one drug, tell your doctor. You might be at risk for similar ones.
- Ask if genetic testing is available for your drug-especially if you’re of Asian descent or taking anticonvulsants, antibiotics, or antiretrovirals.
Final Thought
Idiosyncratic drug reactions will never be fully predictable. The human immune system is too complex. But we’re no longer helpless. With better science, smarter screening, and more awareness, we’re learning how to spot them faster-and avoid them before they strike.The goal isn’t to eliminate all risk. It’s to turn the unknown into the known. One gene, one test, one patient at a time.






Comments
Alec Stewart Stewart
3 February 2026Man, I had no idea meds could mess you up like this. My cousin took that antibiotic for a sinus infection and ended up in the ICU with a rash that looked like she’d been burned. Took weeks to figure out it was the drug. Glad they’re finally testing for this stuff now. 🙏
Demetria Morris
5 February 2026It’s irresponsible that pharmaceutical companies still push drugs without proper immune profiling. People are dying because corporations prioritize profit over prevention. This isn’t just bad luck-it’s systemic negligence. We need accountability, not just ‘awareness.’
Susheel Sharma
7 February 2026Let’s be brutally honest: this is the cost of over-medicalization. We’ve turned every sniffle into a prescription opportunity. The body isn’t a machine to be tinkered with-it’s a delicate ecosystem. When you force chemicals into it, you’re playing Russian roulette with your immune system. 🎯
Janice Williams
8 February 2026It is profoundly disturbing that individuals continue to self-administer pharmaceuticals without comprehensive genetic screening. The onus must shift from reactive diagnostics to preemptive genomic interrogation. This is not a matter of personal responsibility-it is a failure of public health infrastructure.
Roshan Gudhe
9 February 2026There’s something poetic about how medicine, meant to heal, sometimes becomes the very thing that breaks us. We think we’ve tamed biology with science, but the body remembers what our labs forget. Maybe the real breakthrough isn’t in genes or tests-but in humility. We don’t control the immune system. We just beg it to tolerate us.
Rachel Kipps
10 February 2026i never knew about the rucam scale or alden score… this is so important. my mom had liver issues after a painkiller and they thought it was gallstones for months. if only someone had asked about timing…
Alex LaVey
11 February 2026Just want to say thank you for writing this. I had DRESS syndrome from an antibiotic back in 2018. No one believed me until my hands started peeling. Now I’m healthy, but I still get panic attacks when I see a new prescription. Knowledge saves lives. Keep sharing this.
Jhoantan Moreira
11 February 2026Wow. This is one of the clearest explanations I’ve ever read on IDRs. The HLA gene examples alone should be mandatory reading for every med student. 🙌 The fact that we’re now using AI to predict these reactions? That’s the future we need-smart, safe, and science-driven.
Justin Fauth
12 February 2026Y’all in the US are lucky. In India, they sell antibiotics like candy at corner stores. No prescription. No lab tests. No idea what’s in the pill. People die from this every week and no one even blinks. This isn’t a medical issue-it’s a cultural disaster.
Meenal Khurana
12 February 2026Stop the drug. That’s it.