Medication Absorption Calculator
How Your Gut Affects Medications
Calculate how food, fiber, and GI conditions impact your medication absorption based on real research from the article.
Most people think taking a pill is simple: swallow it, wait, and feel better. But for many, that’s not how it works. If you’ve ever taken a medication and wondered why it didn’t help-even when you followed the instructions exactly-you’re not alone. The real issue often isn’t the drug itself. It’s whether your body could absorb it at all.
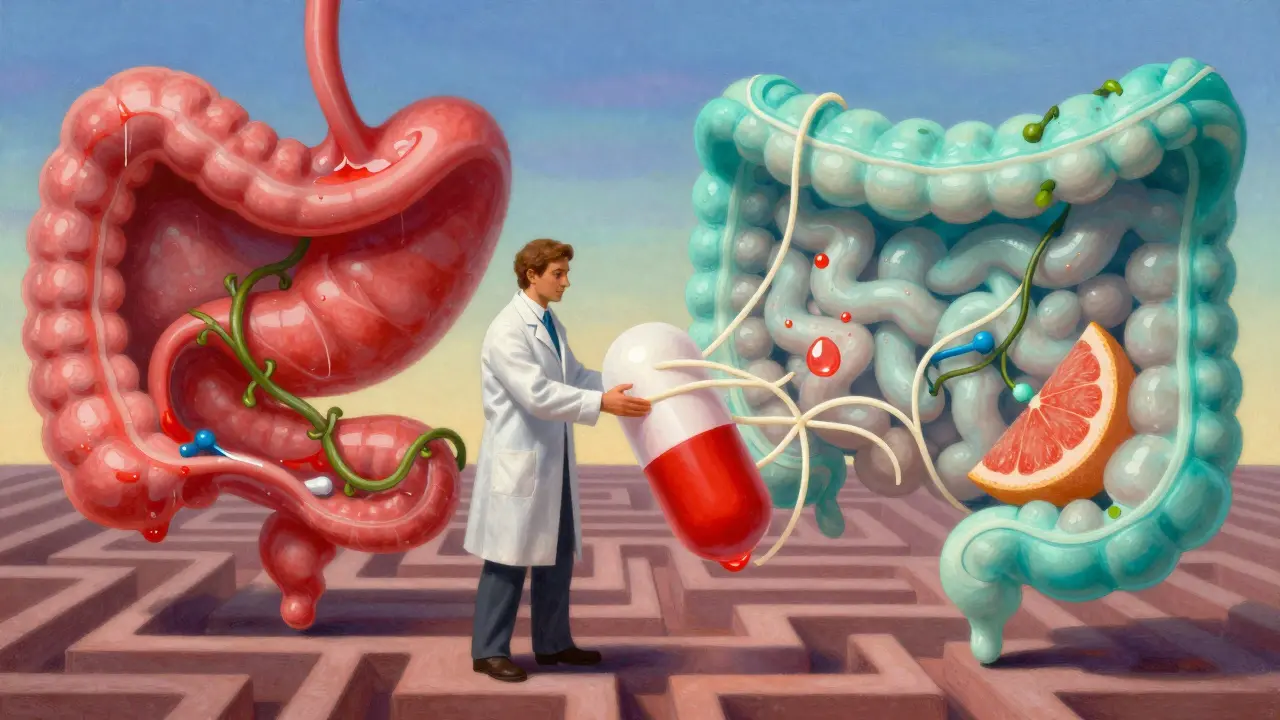
Why Your Stomach and Intestines Block Your Medication
Your digestive system isn’t designed to let drugs slip through easily. It’s built to protect you. The stomach’s acid, the thick mucus lining your gut, enzymes that break down foreign substances, and tight junctions between intestinal cells all act like checkpoints. These barriers keep harmful bacteria and toxins out. But they also stop many medications from getting into your bloodstream where they need to go.Only about 20% of oral drugs make it past these defenses without help. For some, like insulin or large biologic drugs, absorption is near zero without special delivery systems. Even common drugs like levothyroxine, used for thyroid problems, can lose effectiveness if taken with food. A fatty meal can delay gastric emptying by up to four hours, cutting peak drug levels by half. That’s why doctors tell you to take it on an empty stomach-because your gut is working against the drug otherwise.
The pH Game: Where Your Drug Gets Stuck
The pH in your gut changes as you move from stomach to intestine. Your stomach is acidic (pH 1.5-3.5), ideal for breaking down food but terrible for many drugs. As you reach the small intestine, pH rises to around 6-8. That shift matters because drugs need to be in their uncharged form to cross cell membranes. Acidic drugs like aspirin dissolve better in the stomach. Basic drugs like amoxicillin work better in the higher pH of the small intestine.But here’s the catch: if your gut moves too fast-like in diarrhea-or too slow-like in constipation-the drug doesn’t spend enough time in the right spot to be absorbed. That’s why people with irritable bowel syndrome (IBS) often report inconsistent results from the same meds. One day they feel relief, the next day nothing. It’s not them. It’s their gut timing.
Food, Fiber, and the Hidden Saboteurs
You might think eating with your meds helps them absorb better. Sometimes it does. But often, it backfires. Fats slow down how fast your stomach empties. That’s good for some drugs, bad for others. For example, the cholesterol drug atorvastatin absorbs better with food, while the antibiotic ciprofloxacin absorbs worse. Grapefruit juice? It blocks enzymes that break down over 85 medications, including some blood pressure pills and statins, leading to dangerous spikes in blood levels.Even fiber can interfere. High-fiber diets, while healthy, can bind to drugs like digoxin or thyroid meds, trapping them in the gut instead of letting them enter the bloodstream. One study showed that people eating a high-fiber breakfast had 30% lower absorption of levothyroxine compared to those who took it alone. That’s the difference between being in range and needing a dose increase.
When Your Disease Breaks Your Absorption
If you have Crohn’s disease, ulcerative colitis, or short bowel syndrome, your body’s ability to absorb drugs isn’t just slowed-it’s broken. Inflammation damages the intestinal lining. Scar tissue reduces surface area. Surgeries remove parts of the intestine where absorption normally happens.Take mesalamine, a drug used to treat inflammatory bowel disease. In healthy people, it absorbs well. In someone with severe ulcerative colitis, absorption drops by 25-40%. That means the drug meant to calm inflammation never reaches the inflamed areas. Patients report flare-ups despite taking their pills regularly. Pharmacists see this too: INR levels in people on warfarin swing wildly in IBD patients, not because they’re inconsistent, but because their gut can’t absorb the drug consistently.
People with short bowel syndrome often need two to three times the normal dose of antibiotics or vitamins just to reach therapeutic levels. And even then, it’s not guaranteed. Fat-soluble vitamins like D and K? They’re nearly impossible to absorb without enough small intestine. That’s why many of these patients need injections instead of pills.
What Happens When Your Drug Gets Metabolized Before It Even Starts
Even if a drug makes it past the gut lining, it doesn’t escape unscathed. The liver gets the first shot at breaking it down. This is called first-pass metabolism. For some drugs, like propranolol or nitroglycerin, up to 90% is destroyed before it ever reaches your bloodstream. That’s why some medications come as patches, sprays, or injections-they bypass the liver entirely.And then there are drug interactions. GLP-1 agonists like semaglutide (Ozempic, Wegovy) slow down gut movement. That sounds helpful for weight loss, but it’s a problem if you’re also taking a blood thinner or seizure medication. Slower transit means more time for the drug to sit in your gut, but also more chance for it to be degraded or absorbed too slowly. Studies show these drugs can reduce absorption of other meds by 15-30%. That’s enough to make a life-saving drug ineffective.
Why Your Pill Might Not Be the Problem
It’s not just what’s inside the pill. It’s how it’s made. A tablet can be designed to dissolve slowly, quickly, or only in the colon. But if your gut is inflamed, the coating might break open too early-or not at all. Asacol HD, a delayed-release mesalamine, is meant to release in the colon. But if your colon is too inflamed, the coating dissolves prematurely, and the drug gets absorbed too soon-before it reaches the target.Formulation matters. Some drugs come as powders, liquids, or chewables for people who can’t swallow pills. Children, elderly patients, and those with swallowing issues often need these forms. But even then, if the liquid is mixed with juice or milk, absorption can drop. Pharmacists know this. They’ve seen patients take their liquid antibiotics with orange juice and wonder why they’re still sick.
What’s Being Done to Fix This
Pharmaceutical companies are finally paying attention. New formulations use nanoparticles, liposomes, or fat-based carriers to help drugs sneak through the gut lining. Some additives-like sodium caprate or chitosan-can temporarily open tight junctions to let drugs pass. These enhancers have boosted absorption by 20% to 200% in trials.Doctors are starting to use models that simulate how a drug behaves in a diseased gut. These aren’t just lab tricks-they predict real outcomes. The FDA now requires drug developers to test new oral meds in models that mimic Crohn’s or IBS. That’s a big step. Still, only 15-20% of current oral drugs have clear dosing instructions for patients with GI diseases. Most labels say nothing.
Future tech might include smart pills with sensors that measure pH, pressure, and transit time inside your gut. Imagine a pill that tells your doctor exactly where and when your drug was absorbed-and adjusts your next dose automatically. Early trials are already underway.
What You Can Do Right Now
If you’re on long-term GI meds and feel like they’re not working:- Take them exactly as directed-on an empty stomach, with water, not juice.
- Keep a log: when you took the drug, what you ate, and how you felt. Patterns matter.
- Ask your pharmacist: Is this drug affected by food, fiber, or other meds you take?
- If you have IBD or a gut surgery, ask if your drug has special dosing guidelines for your condition.
- Don’t switch brands without checking. Generic versions may have different coatings or fillers that change absorption.
There’s no one-size-fits-all fix. But understanding that your gut isn’t just a pipe-it’s a complex, changing system-gives you power. You’re not failing your treatment. Your body is. And now, you know why.







Comments
Virginia Seitz
16 December 2025So basically my thyroid med is just a fancy rock I swallow? 😅 Thanks for confirming my 3-year struggle wasn't just me being lazy. I take it with coffee now. Oops.
Pawan Chaudhary
17 December 2025This is so helpful! I’ve been taking my meds with breakfast for years thinking it’d help. Now I know why I still feel tired. Gonna switch to water only and keep a log. Thank you for explaining it so clearly 🙏
Linda Caldwell
18 December 2025Stop blaming your gut and start blaming Big Pharma. They don’t want you to absorb meds properly. They want you coming back every month. It’s all about the profit. The system is rigged. I’ve seen the documents.
Chris Van Horn
20 December 2025While your exposition is superficially coherent, it fundamentally misrepresents the pharmacokinetic architecture of gastrointestinal absorption. The notion that 'only 20% of oral drugs make it past these defenses' is a gross oversimplification derived from outdated in vitro models that fail to account for dynamic enteric recycling, efflux transporter polymorphisms, and microbiome-mediated biotransformation. The real issue lies in the underappreciated role of P-glycoprotein expression gradients along the jejunoileal axis - a variable systematically ignored in clinical guidelines. Furthermore, your dismissal of formulation science is egregious. Enteric-coated microspheres with pH-dependent dissolution profiles, when coupled with bile salt-mediated micellar solubilization, can achieve bioavailability exceeding 85% in IBD patients - provided the disease activity is stratified. Your anecdotal references to 'grapefruit juice' and 'fiber binding' are pedagogically useful but statistically insignificant in the context of population-level PK/PD modeling. You have, in essence, reduced a multidimensional pharmacological problem to a dietary checklist. This is not enlightenment. It is pharmaceutical reductionism.
BETH VON KAUFFMANN
20 December 2025TL;DR: Your gut is a picky eater and Big Pharma doesn’t care. The real issue? No one’s been held accountable for designing drugs that assume a healthy GI tract. We’ve got 80% of chronic meds built for a 1970s ideal patient - white, middle-class, no comorbidities, no meds, no stress. Meanwhile, 60% of the population has some form of dysmotility, inflammation, or dysbiosis. We’re just supposed to ‘take it on an empty stomach’ and hope for the best? This isn’t medicine. It’s guesswork with a prescription pad.
Steven Lavoie
22 December 2025Chris Van Horn’s comment is technically correct but misses the human point. The article isn’t about P-glycoprotein polymorphisms - it’s about people who feel fine one day and collapsed the next, not because they’re noncompliant, but because their body’s environment changed. That’s why the advice to log meals and timing matters. Real medicine isn’t just about molecules - it’s about context. I’ve seen patients on warfarin with IBD whose INR swings 3 points in a week. No one told them to check if their fiber intake changed. This article gives them the language to speak up. That’s valuable.
Victoria Rogers
23 December 2025So now I’m supposed to believe the government and pharma are hiding the truth? That’s why my blood pressure meds don’t work. It’s not me. It’s the gut. And the gut is controlled by the elites. I read a guy on Telegram who said they add anti-absorption agents to pills to keep us docile. I’m not taking anything until I get it compounded with no fillers. And no, I won’t tell you my meds. You’re probably on their payroll.
Jonathan Morris
25 December 2025There’s a smart pill being tested that tracks absorption. I’ve seen the patent filings. It’s not for patients. It’s for insurance companies to track compliance and deny refills if your gut ‘didn’t absorb enough.’ They’re building a surveillance system disguised as innovation. Don’t be fooled. This isn’t progress. It’s control.