Warfarin INR Stability Calculator
Your INR History
Enter your last 10 INR values (normal range: 1.5-4.0)
Vitamin K Intake
Your INR Stability Report
Stability Score
INR Range: 1.5 - 4.0 (Therapeutic Range)
Current INR: -
What Your Score Means
If you're on warfarin, you know how unpredictable your INR levels can be. One week you're perfect, the next you're bleeding or clotting, and your doctor keeps changing your dose. It’s exhausting. But what if the problem isn’t your warfarin dose at all? What if it’s your vitamin K intake?
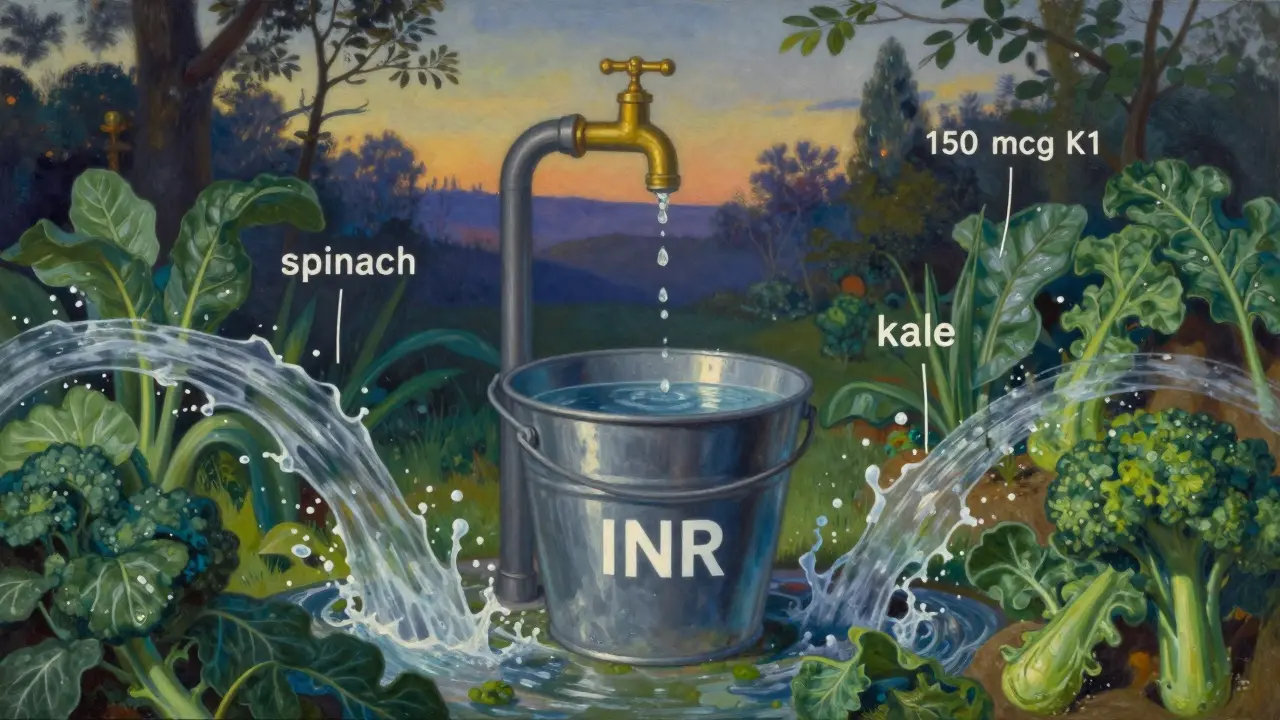
Why Your INR Fluctuates
Warfarin works by blocking vitamin K from helping your blood clot. That’s why it prevents dangerous clots. But here’s the catch: vitamin K isn’t just in supplements. It’s in spinach, kale, broccoli, Brussels sprouts, and even some oils. One day you eat a big salad, your INR drops. The next day you skip greens, your INR spikes. That’s why so many people on warfarin have unstable INR levels-between 30% and 50% of them, according to the American Heart Association.It’s not about eating too much or too little vitamin K. It’s about inconsistency. Your body needs a steady amount. If you’re swinging between 50 mcg one day and 500 mcg the next, your warfarin dose can’t keep up. That’s where low-dose vitamin K supplementation comes in-not to fight warfarin, but to smooth out the ride.
The 150 mcg Solution
Research shows that taking 150 micrograms (mcg) of vitamin K1 daily can make a real difference. That’s about 1.5 times the daily recommended intake for adults, but still far below any toxic level. This dose doesn’t change your warfarin’s effect-it just gives your body a consistent baseline.A 2007 study in Blood found that patients who took 150 mcg daily had much more stable INR levels than those who didn’t. Their INR swings dropped by nearly half. Another study in 2016, done across Canadian clinics, confirmed it: patients on vitamin K supplements had 4% fewer dangerous INR spikes (above 4.0) or crashes (below 1.5). That might sound small, but in real terms, it means one fewer emergency visit per patient per year.
This isn’t magic. It’s physics. Think of your INR like water in a bucket. Warfarin is the drain. Vitamin K from food is the faucet-sometimes it’s wide open, sometimes it’s dripping. Adding a steady drip of 150 mcg vitamin K every day? That’s like installing a small, constant trickle. Now the water level stays even, even if the faucet changes.
Who Benefits Most
Not everyone on warfarin needs this. If your INR is consistently between 2.0 and 3.0, you’re fine. But if you’re one of the 30-50% with wild swings, and you’ve already tried eating the same amount of greens every day, this might be your next step.Good candidates usually have:
- TTR (Time in Therapeutic Range) under 65% over six months
- Three or more INR values above 4.0 or below 1.5 in the past year
- No major dietary changes (like suddenly eating a lot of kale)
- No mechanical heart valves in the mitral position (those need higher INR targets)
People with kidney disease on dialysis, or those with antiphospholipid syndrome, often benefit the most. Their bodies handle vitamin K differently, and warfarin becomes extra unpredictable.
What Happens When You Start
Don’t expect instant results. It takes 4 to 8 weeks for your INR to settle. In the first two weeks, your INR might actually drop. That’s normal. Your body is adjusting to the steady vitamin K. Your doctor will likely increase your warfarin dose slightly-by 0.5 to 1.5 mg-to compensate. In one study, the average warfarin dose went from 4.8 mg to 5.4 mg daily after starting vitamin K.Monitoring stays critical. You’ll still need weekly INR checks for the first month, then every two weeks. Don’t assume you’re stable just because you’re taking vitamin K. The goal isn’t to stop testing-it’s to make your test results less scary.
What It Doesn’t Do
Vitamin K won’t fix everything. If you’re skipping your warfarin pills, it won’t help. If you’re suddenly eating a whole head of kale every day, it won’t help. If you’re on a new antibiotic or herbal supplement that interferes with warfarin, it won’t help. It’s not a band-aid. It’s a tool for people who are already doing everything right-except keeping their vitamin K steady.It also doesn’t replace DOACs like apixaban or rivaroxaban. Those drugs don’t need INR monitoring at all. But for people with mechanical heart valves or certain clotting disorders, warfarin is still the only option. That’s where vitamin K supplementation shines.
Cost and Accessibility
This is one of the cheapest interventions in medicine. A 5 mg bottle of vitamin K1 (phylloquinone) costs about $8 at Walgreens. That’s 100 tablets. You only need 150 mcg per day-that’s one-third of a tablet. So you’re paying less than half a cent per day.It’s available over the counter. No prescription needed. But don’t just buy any supplement. Look for phylloquinone (vitamin K1), not menaquinone (K2). K2 doesn’t work the same way with warfarin. And avoid multivitamins with high doses of K-stick to the 150 mcg dose.
What Doctors Say
Some doctors are hesitant. The American College of Chest Physicians says the evidence isn’t strong enough for a formal recommendation. But others are convinced. Dr. Jacob Siegel at Johns Hopkins says the 4% drop in dangerous INR excursions means about 15 fewer high-risk readings per patient each year. That’s enough to prevent strokes or major bleeds.Dr. Elaine Hylek from Boston University calls it “one of the most promising approaches” to warfarin stability. And in Europe, the 2020 Heart Rhythm Association guidelines give it a “may be considered” recommendation-Class IIb, Level B.
The big shift is coming. In 2023, the American Heart Association added vitamin K supplementation to its “promising practices” list for warfarin patients. If results from the ongoing VIKING trial (expected late 2024) confirm the benefits, this could become standard care by 2026.
Real Patient Stories
One man, 68, with a mechanical aortic valve, had an INR TTR of just 42% over 18 months. He was constantly adjusting his warfarin. After starting 150 mcg vitamin K daily, his TTR jumped to 71% in six months. He needed only two dose changes instead of 17.Another patient, on Reddit, said her INR was a rollercoaster for eight years. After vitamin K, her TTR went from 55% to 78%. She went from 11 INRs over 4.0 in six months to just two.
But not everyone wins. Some patients see no change. A few even get worse. That’s why it’s not for everyone. If your INR doesn’t improve after three months, stop it. There’s no point forcing it.
How to Start
If you think this might help you:- Track your INR for six months. If your TTR is below 65%, talk to your hematologist or anticoagulation clinic.
- Ask if they’ve used vitamin K supplementation before. Most clinics now have protocols.
- If they agree, get 150 mcg of phylloquinone (vitamin K1). Buy it as a standalone tablet, not in a multivitamin.
- Take it at the same time every day-preferably with food, since it’s fat-soluble.
- Keep your diet consistent. Don’t suddenly start eating a lot of greens or stop.
- Stick to your INR checks. Don’t skip them, even if you feel fine.
And if your doctor says no? Ask why. If it’s because “there’s no evidence,” show them the 2016 Canadian trial or the 2022 systematic review in Blood Advances. This isn’t fringe science anymore. It’s becoming standard.
The Bigger Picture
Warfarin is old, but it’s not going away. Over 2 million Americans still rely on it. And for many, it’s the only option. Vitamin K supplementation doesn’t replace it. It makes it work better.It’s not about taking more of something. It’s about taking the right amount, every day. That’s the secret to stable INR. Not luck. Not guesswork. Just consistency.
If you’ve been stuck in the warfarin rollercoaster, this might be your way off. But only if you’re ready to make it part of your routine-every day, without fail.
Can I take vitamin K supplements while on warfarin?
Yes, but only under medical supervision. A consistent daily dose of 150 mcg of vitamin K1 (phylloquinone) can help stabilize INR levels in people with unexplained fluctuations. It’s not a substitute for warfarin, but it helps your body respond more predictably to it. Never start without talking to your doctor.
Does vitamin K lower INR?
Yes, vitamin K counteracts warfarin’s effect, which can lower INR. But when taken daily at 150 mcg, it doesn’t cause dangerous drops-it smooths out the highs and lows. Your doctor will adjust your warfarin dose accordingly. The goal isn’t to make your INR lower, but to keep it steady.
What’s the best time to take vitamin K with warfarin?
Take it at the same time every day, preferably with a meal that contains some fat-like eggs, nuts, or olive oil. Vitamin K is fat-soluble, so it absorbs better with food. Consistency matters more than the exact time. Just pick a time and stick to it.
Can I get enough vitamin K from food instead of supplements?
Possibly, but it’s hard. Foods like kale, spinach, and broccoli have high vitamin K, but their levels vary by season, cooking method, and brand. One cup of raw spinach has about 145 mcg, but cooked has over 800 mcg. That’s too much variation. Supplements give you a precise, consistent dose-something food can’t reliably do.
How long does it take for vitamin K to stabilize INR?
It usually takes 4 to 8 weeks. In the first few weeks, your INR might drop as your body adjusts. Don’t panic. Your doctor will monitor and adjust your warfarin dose. Stability improves gradually. Don’t expect overnight results.
Are there side effects from taking vitamin K with warfarin?
At 150 mcg daily, side effects are extremely rare. Vitamin K1 is safe at this dose-even long-term. The main risk isn’t from the supplement itself, but from stopping INR monitoring. If you assume you’re stable and skip blood tests, you could miss a dangerous change. Always keep your appointments.
Should I take vitamin K if I have a mechanical heart valve?
Yes, but only if your INR is unstable. People with mechanical heart valves often need higher INR targets (2.5-3.5), and they’re more prone to fluctuations. Studies show vitamin K supplementation helps even in this group-especially if your INR keeps drifting out of range despite consistent dosing. But always work with your cardiologist or anticoagulation clinic.
What if vitamin K doesn’t work for me?
If your INR doesn’t improve after 3 months, stop the supplement. It’s not for everyone. You might have another issue-poor warfarin adherence, drug interactions, or liver problems. Your doctor can investigate further. Don’t keep taking it hoping it’ll work. There are other options, including switching to a DOAC if you’re eligible.
Can I take vitamin K with other medications?
Most common medications are fine. But antibiotics, antifungals, and some seizure drugs can interfere with warfarin. Vitamin K won’t fix those interactions. Always tell your doctor about every pill, herb, or supplement you take. Some herbs like ginseng, green tea, and St. John’s wort can affect your INR too.
Is vitamin K supplementation covered by insurance?
Usually not, because it’s sold as a supplement, not a prescription drug. But it costs less than $0.01 a day. Most people pay out of pocket. The real cost savings come from fewer hospital visits, emergency INR checks, and bleeding events. That’s why many anticoagulation clinics recommend it-even if insurance won’t pay for it.




Comments
Gina Beard
23 January 2026Consistency is the quiet hero of anticoagulation. Not the big changes. Not the frantic dose tweaks. Just the same 150 mcg, same time, every day. Like brushing your teeth. No drama. Just presence.
Don Foster
23 January 2026Look i've seen this study cited 3x in the last month and its still just a pilot with n=120 and no long term safety data the aha says 'promising practices' not 'standard of care' and if you think 150 mcg is safe for everyone you're ignoring the fact that k1 can accumulate in hepatic tissue over time and fuck with vitamin k dependent proteins beyond coagulation like osteocalcin and matrix gla protein so stop treating this like a magic bullet its not
Phil Maxwell
23 January 2026My dad started this after his 4th hospital visit for a bleed. Took him 6 weeks to stabilize. Now his INR is the most consistent its been in 7 years. He still checks weekly. Still sees his doc. But the panic? Gone. It’s not perfect. But it’s the first thing that actually made sense.
Shelby Marcel
25 January 2026wait so u just take like 1/3 of a tablet? how do u even cut it?? i tried splitting a 5mg tab with a knife and it just exploded into dust lol
blackbelt security
26 January 2026If you’re on warfarin and your INR is a rollercoaster, this isn’t a suggestion. It’s a survival hack. Do the work. Take the pill. Track your numbers. Don’t wait for a crisis to start being smart.
Patrick Gornik
26 January 2026Here’s the uncomfortable truth no one wants to say: warfarin is a 1940s relic held together by duct tape and wishful thinking. Vitamin K1 at 150 mcg isn’t a supplement-it’s a *protocol adjustment* to compensate for the pharmacokinetic chaos of a drug designed before we understood epigenetics. The real scandal? We’re still using this archaic anticoagulant because the pharmaceutical industry has zero incentive to replace it with DOACs for mechanical valve patients. This isn’t innovation. It’s damage control dressed up as biohacking. But hey, if it keeps you out of the ER, who am I to judge the aesthetics of your pharmacological patchwork?
asa MNG
28 January 2026OMG YES I DID THIS AND MY INR WENT FROM 1.8 TO 5.2 IN 3 DAYS 😱 I THOUGHT I WAS GONNA DIE BUT MY DR SAID IT WAS NORMAL?? I TOOK VIT K 150 MCG BUT I ALSO ATE A WHOLE BAG OF SPINACH THAT DAY 😭 I THINK I DID IT WRONG BUT NOW IM ADDICTED TO THE STABILITY 😍 #warfarinlife #vitamink1savior
Tiffany Wagner
29 January 2026I’ve been on warfarin for 12 years. Tried everything. This is the first thing that actually made my numbers feel human. I take mine with my morning coffee and a spoon of peanut butter. No drama. Just steady. I’m not a fan of supplements but this one? Worth it.