Understanding Juvenile Arthritis: An Overview
Juvenile arthritis is a term used to describe a group of chronic, inflammatory conditions that affect children and adolescents. These conditions can cause joint pain, swelling, stiffness, and reduced mobility, significantly impacting the daily lives of those affected. In this article, we will explore the different types of juvenile arthritis and their characteristics, so that you can better understand the challenges faced by children and adolescents living with these conditions.
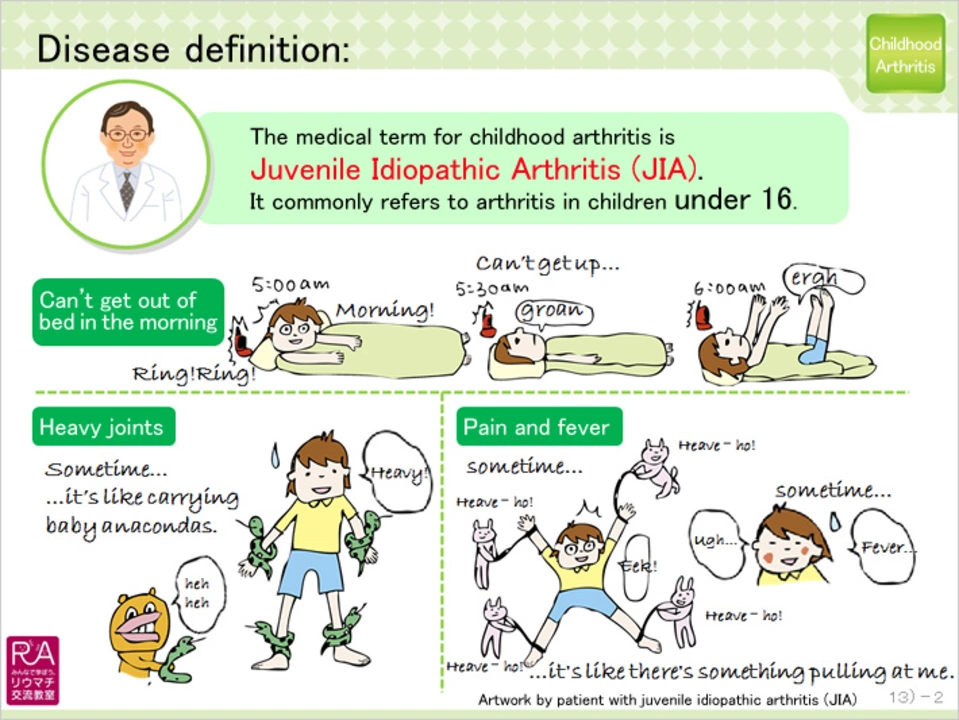
1. Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) is the most common form of juvenile arthritis, accounting for approximately 75% of cases. It is characterized by joint inflammation that lasts for at least six weeks and typically begins before the age of 16. JIA can be further divided into several subtypes, each with its own unique characteristics:
a. Oligoarticular JIA
Oligoarticular JIA, also known as pauciarticular JIA, is the most common subtype, affecting around 50% of children with JIA. This form involves inflammation in four or fewer joints, usually in the knees, ankles, or wrists. Oligoarticular JIA tends to have a milder course, with less severe symptoms and a better overall prognosis compared to other subtypes.
b. Polyarticular JIA
Polyarticular JIA affects around 30% of children with JIA and is characterized by inflammation in five or more joints. This subtype can be further divided into two groups - rheumatoid factor (RF) positive and RF negative. RF-positive polyarticular JIA is more similar to adult rheumatoid arthritis and tends to have a more aggressive course, with a higher risk of joint damage and disability. On the other hand, RF-negative polyarticular JIA has a more variable course, with some children experiencing mild symptoms and others having more severe disease progression.
c. Systemic JIA
Systemic JIA, also known as Still's disease, affects around 10% of children with JIA and is characterized by inflammation not only in the joints but also in other organs, such as the heart, lungs, and liver. This subtype is associated with high fevers, rash, and swollen lymph nodes, and can be more difficult to treat compared to other forms of JIA.
2. Juvenile Lupus
Juvenile lupus is an autoimmune disease that affects various organs and systems in the body, including the joints, skin, kidneys, and blood vessels. Joint involvement in juvenile lupus can be similar to JIA, with pain, swelling, and stiffness being common symptoms. However, the presence of other symptoms, such as a butterfly-shaped rash on the face, mouth ulcers, and kidney problems, can help distinguish juvenile lupus from JIA. Treatment for juvenile lupus typically involves medications to suppress the immune system and reduce inflammation, as well as lifestyle modifications to manage symptoms and prevent complications.
3. Juvenile Dermatomyositis
Juvenile dermatomyositis is a rare autoimmune disease that affects the muscles and skin, resulting in muscle weakness and a characteristic rash. While joint involvement is less common in juvenile dermatomyositis compared to other forms of juvenile arthritis, some children may experience arthritis-like symptoms, such as joint pain and stiffness. Treatment for juvenile dermatomyositis typically includes medications to suppress the immune system, as well as physical therapy and occupational therapy to help maintain muscle strength and function.
4. Juvenile Scleroderma
Juvenile scleroderma is another rare autoimmune disease that affects the connective tissues in the body, causing thickening and hardening of the skin. In some cases, joint involvement may also occur, leading to pain, stiffness, and reduced mobility. There are two main types of juvenile scleroderma - localized and systemic. Localized scleroderma primarily affects the skin, whereas systemic scleroderma can also involve internal organs. Treatment for juvenile scleroderma may include medications to suppress the immune system, as well as physical and occupational therapy to help manage symptoms and maintain function.
5. Juvenile Psoriatic Arthritis
Juvenile psoriatic arthritis is a subtype of JIA that is associated with the skin condition psoriasis. Children with juvenile psoriatic arthritis typically experience joint inflammation, as well as skin symptoms such as red, scaly patches on the skin. Treatment for juvenile psoriatic arthritis typically involves medications to reduce inflammation and suppress the immune system, as well as skin treatments to manage psoriasis symptoms.
In conclusion, juvenile arthritis encompasses a range of chronic, inflammatory conditions that affect children and adolescents. While each type of juvenile arthritis has its own unique characteristics, the common thread is joint involvement, leading to pain, stiffness, and reduced mobility. By better understanding the different types of juvenile arthritis and their characteristics, we can work towards improving the lives of those affected by these conditions through early diagnosis, effective treatment, and ongoing support.






Comments
Steven Young
2 June 2023The whole JIA narrative is just another pharma ploy to push drugs onto unsuspecting families
Holly Green
2 June 2023We have a duty to protect kids from unnecessary medication. The information here is thorough but families need clear guidance. I appreciate the balanced overview.
Craig E
2 June 2023It’s heart‑warming to see such comprehensive detail laid out for caregivers. While the clinical terminology can feel dense, the underlying compassion shines through. One can almost hear the whispered hopes of parents yearning for relief. The distinctions among subtypes remind us that each child’s journey is uniquely colored. Let us remember that knowledge, when paired with empathy, becomes a beacon in the fog of uncertainty.
Marrisa Moccasin
2 June 2023Honestly, the "official" narrative is riddled with hidden agendas, you can see it everywhere-big pharma, government labs, and even the so‑called "experts"-they all want you to believe that these classifications are purely scientific, but the truth is masked, by layers of PR, and controlled studies, that never reveal the real side‑effects!
Caleb Clark
2 June 2023Hey everyone, I just wanted to throw out some encouragement for all the families out there battling juvenile arthritis-this is a tough road but you are not alone, okay? First, remember that early diagnosis can really make a difference, so keep pushing for those thorough check‑ups even if the doc seems rushed, because every extra week of uncontrolled inflammation can set back growth and joint function. Second, physical therapy isn’t just a fancy extra, it’s a cornerstone of maintaining mobility and muscle strength-yes, the sessions can be tiring, but the long‑term payoff in range of motion is worth every sore day. Third, don’t underestimate the power of a balanced diet, packed with omega‑3 fatty acids and anti‑inflammatory foods; I’ve seen kids improve their pain levels just by tweaking their meals, even though it takes patience to change old habits. Fourth, stay on top of medication schedules-some of the newer biologics have incredible results, but you’ve gotta be mindful of side‑effects, and always report anything weird to your rheumatologist, even if it seems minor, because catching issues early can prevent bigger problems later. Fifth, mental health matters big time-dealing with chronic pain can lead to anxiety and depression, so consider counseling or support groups; sharing experiences can lighten the emotional load and give you practical tips you wouldn’t otherwise find. Sixth, keep a symptom journal, details like flare timing, activity levels, and food intake can help your medical team fine‑tune treatments, and honestly, writing it down can give you a sense of control. Seventh, never hesitate to ask for second opinions; a fresh set of eyes on a complex case can uncover alternative therapies or clinical trials that might be a better fit. Eighth, celebrate small victories-whether it’s a day without swelling or a new milestone in school, those wins build confidence and keep morale high. Ninth, involve the whole family in care plans; when siblings understand what’s happening, they become allies rather than sources of stress. Finally, remember that research is constantly evolving-new drugs and biomarkers are on the horizon, so staying informed through reputable sources can give you hope for even better outcomes in the future. You’ve got a community behind you, and together we can navigate this challenging journey with resilience and optimism.
Eileen Peck
3 June 2023I totally agree with the supportive tone, and I’ve seen the benefits of journaling in my own practice-sometimes the tiniest notes can guide big decisions. Also, don’t forget that every child’s response is unique, so flexibility is key. If you ever need more resources, I’m happy to share some reliable links.
Oliver Johnson
3 June 2023Look, the American healthcare system is the best, and no foreign interference should dictate our treatment protocols. If anyone tries to push alternative approaches, they’re just undermining our superiority.
Taylor Haven
3 June 2023It’s astonishing how easily the public is led to trust the mainstream narrative without questioning the hidden motives behind every study, especially when it comes to chronic conditions like juvenile arthritis. The media, in collusion with pharmaceutical conglomerates, crafts stories that glorify expensive biologics while downplaying natural interventions that could be equally effective. Moreover, the FDA’s rapid approvals often bypass rigorous long‑term safety data, putting vulnerable children at risk for unknown side‑effects. Parents are constantly bombarded with glossy advertisements promising miracles, yet they receive little transparent information about potential risks. Governments, fearful of losing control, impose regulations that stifle independent research, ensuring that only the approved, profit‑driven treatments dominate the market. It’s a systematic effort to keep the population dependent on a cycle of medication, monitoring, and endless follow‑ups. When you look at the data, the surge in diagnosis rates aligns suspiciously with pharmaceutical lobbying spikes. This isn’t a coincidence; it’s a calculated strategy to expand the customer base. Communities must demand true transparency and support grassroots research that prioritizes patient well‑being over corporate profit.
Jonathan Harmeling
3 June 2023While the discourse here is certainly spirited, let’s not overlook the fact that many of these medical advances have genuinely improved quality of life-though, of course, a little extra scrutiny never hurts.