When a life-saving medication disappears from the pharmacy shelf, patients don’t just lose a pill-they lose stability, trust, and sometimes hope. Drug shortages aren’t rare anymore. In 2023, nearly 300 medications were in short supply in the U.S., from heart drugs to cancer treatments. And when this happens, the responsibility doesn’t end with the manufacturer or the pharmacist. Healthcare providers are on the front line of keeping patients safe, informed, and calm.
Why communication isn’t optional
Patients don’t ask for updates because they’re curious. They’re scared. A 2023 study found that 73% of patients lose trust in their provider if they hear about a drug shortage from someone else-like a pharmacist or a friend-before their doctor says anything. That’s not just bad customer service. It’s a breach of the therapeutic relationship. The Joint Commission now requires providers to have structured communication plans in place by January 2025. Failure to comply could risk hospital accreditation. But even before that rule, research showed communication failures contributed to 70% of serious medical errors during shortages. Why? Because when patients don’t understand why their medication changed, they skip doses, mix pills, or stop treatment entirely.What providers must tell patients
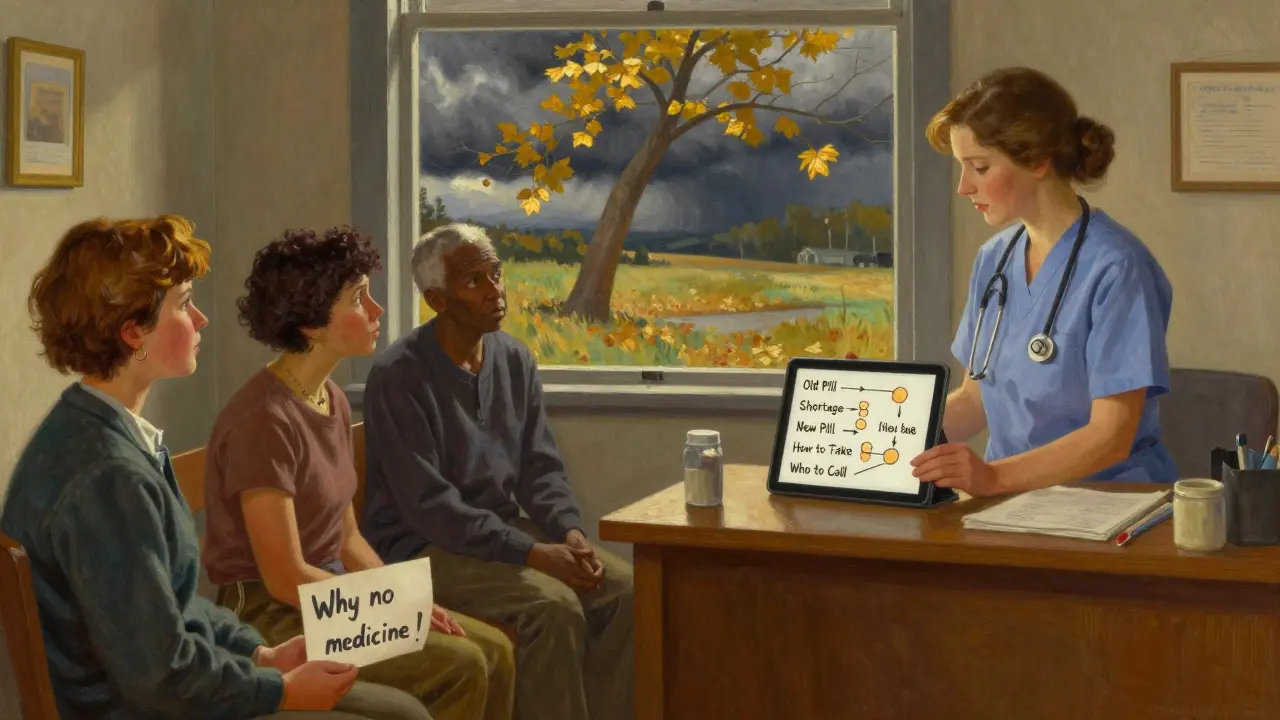
Effective communication during a shortage isn’t about giving a quick update. It’s about giving clear, complete, and compassionate information. The European Medicines Agency’s 2022 guidelines lay out exactly what patients need to know:- The exact name of the medicine (brand and generic)
- Why it’s unavailable (even if the reason is vague, like "supply chain issues")
- How long the shortage is expected to last
- What the safe, proven alternative is-and why it works
- How to reach someone if they have questions
Plain language, not medical jargon
Nearly half of U.S. adults have trouble understanding basic health information. That’s not a personal failing-it’s a system failure. When you tell a patient, "We’re switching you from metoprolol tartrate to metoprolol succinate due to a supply chain disruption," you’re not helping. You’re confusing them. The CDC recommends all shortage communication be written at a 6th- to 8th-grade reading level. That means:- "Metoprolol" becomes "your heart medicine"
- "Supply chain disruption" becomes "the company can’t make enough right now"
- "Therapeutic alternative" becomes "a different pill that works the same way"
Check understanding, don’t assume it
Saying "Do you understand?" isn’t enough. Patients often say yes just to end the conversation. The CDC’s "Chunk, Check, Change" method works better:- Chunk: Give one piece of information at a time-no more than three sentences.
- Check: Ask, "Can you tell me in your own words how you’ll take this new medicine?"
- Change: If they get it wrong, explain again differently. Don’t repeat the same words.
What works: Real examples from clinics
At Mayo Clinic, they use a system called SHIP-Shortage Handling and Information Protocol. When a drug runs low, the pharmacy flags it. The EHR auto-sends a reminder to the provider: "Patient on X drug-shortage alert." The provider then has a template to fill out: name, alternative, reason, timeline, contact info. The whole process takes under two minutes. At Kaiser Permanente, shortage alerts are built into routine visit workflows. When a patient comes in for a refill, the system shows: "Your usual medication is currently unavailable. We’ve switched you to Y. Here’s why." No extra appointment needed. Time spent per patient? Just 2.7 minutes. At Memorial Sloan Kettering, cancer patients get a dedicated communication specialist-not a nurse, not a pharmacist-just someone trained to walk them through emotional, high-stakes changes. They handle every shortage discussion for chemotherapy drugs. Result? 83% of patients continue treatment without interruption.What fails: The quiet breakdowns
Rural clinics struggle the most. Sixty-eight percent of providers there say they don’t get real-time shortage updates. One nurse in West Virginia told a patient, "I don’t know why your blood pressure pill is gone. The pharmacy said it’s out of stock. Try this one." The patient stopped taking it. Three weeks later, they had a stroke. Patients with limited English face 3.2 times more confusion. One Spanish-speaking man in Texas was given a new pill without any translated materials. He thought it was a "different strength" and doubled his dose. He ended up in the ER. And then there’s the Reddit thread: "When my heart medication disappeared." Over 1,200 people commented. Seventy-two percent said their provider just handed them a new pill with no explanation. No why. No alternative. No timeline. Just: "Here. Take this."
What patients really want
A survey of 2,400 patients found three things matter most when a drug is unavailable:- 78% need to know why the original drug is gone.
- 72% want proof the alternative works-like a study or data.
- 65% need a realistic timeline for when the original might come back.
What you can do today
You don’t need a fancy system to start doing this right. Here’s your quick checklist:- Check your EHR-does it flag drug shortages? If not, ask your IT team to add it.
- Create a one-page handout for common shortage drugs: old name, new name, why, how to take, who to call.
- Train your staff to use "Chunk, Check, Change" in every shortage conversation.
- Document every discussion: what you said, how the patient responded, whether they understood.
- Use plain language. No jargon. No assumptions.
It’s not just policy-it’s care
Drug shortages aren’t going away. Global supply chains are fragile. Manufacturing delays happen. But how we respond? That’s still in our control. Patients don’t expect miracles. They just want to know they’re not being left behind. When a provider takes the time to explain, to listen, to check understanding-they don’t just prevent errors. They rebuild trust. The next time a medication runs out, don’t just hand over a new prescription. Have a conversation. Because in a shortage, the most important drug isn’t on the shelf. It’s the one you give them: clarity.What should I do if my medication is on shortage?
Don’t stop taking your medicine without talking to your provider. Contact your doctor or pharmacist immediately. Ask: Why is it unavailable? What’s the alternative? Is it safe? Will my insurance cover it? And when might the original be back? Write down the answers. If you’re unsure, ask to speak with a pharmacist or a care coordinator.
Are generic drugs safe substitutes during shortages?
Yes, if your provider recommends them. Generic drugs contain the same active ingredient as brand-name versions and are required by the FDA to work the same way. The difference is often in inactive ingredients-like fillers or coatings-which rarely affect how the drug works. Your provider will choose a generic that’s clinically equivalent and safe for your condition.
Why do some providers give me a new pill without explaining why?
Sometimes it’s because they’re overwhelmed. A typical doctor visit lasts just over 15 minutes, and many EHR systems don’t flag shortages automatically. But that’s not an excuse. Patients have the right to know why their treatment changed. If you’re not given a clear explanation, ask again. Or ask to speak with someone else-like a pharmacist or nurse navigator.
How can I know if my new medication is working?
Ask your provider what signs to watch for. For example, if you’re switched from one blood pressure pill to another, you might need to check your pressure more often for the first few weeks. Ask: "What should I feel? What symptoms should I report? When should I come back?" If you feel worse, dizzy, or confused, contact your provider right away. Don’t wait for your next appointment.
Is there a way to get notified about future shortages?
Yes. The FDA maintains a public Drug Shortage List on its website. You can sign up for email alerts for specific medications. Also, ask your pharmacy if they offer shortage notifications. Some send texts or emails when a drug you take is running low. Don’t wait for your refill to be denied-stay informed ahead of time.

Comments
anggit marga
31 December 2025This whole post is just corporate fluff wrapped in medical jargon
Providers don't need more templates they need more time and more pay
Stop blaming doctors for supply chain chaos caused by greedy pharma CEOs and Chinese factory closures
My cousin in Lagos gets her meds once every 3 months and she's alive
Y'all need to chill
Joy Nickles
31 December 2025Okay but like... have you seen the EHR systems in rural clinics??
They're literally from 2008 and the button to flag shortages is hidden under 3 menus and a pop-up ad for viagra
And don't even get me started on the fact that the pharmacy's shortage alert system sends notifications to the wrong provider 70% of the time
Also I once got a text that said 'metoprolol succinate now available' but it was for my neighbor's prescription
And I'm like... why am I getting this??
Also also my cat has more consistent meds than my insurance-covered heart pills
And the 'chunk check change' method??
What if the patient is deaf??
And what if they're 87 and have dementia??
And what if they're in a 12-minute visit with 3 other patients waiting??
It's not that simple!!
And why is no one talking about the fact that the FDA approves generics but the insurance companies refuse to cover them unless you jump through 17 hoops??
Also I hate the word 'therapeutic' it sounds like a yoga retreat for pills
Also also I cried last week because my blood pressure med was out and I had to drive 45 minutes to a different pharmacy and they didn't even have it and I just sat in my car and ate a granola bar and cried
Also I'm not even mad
Just... tired
Emma Hooper
31 December 2025Oh honey. You’re preaching to the choir, but let me tell you something - the real magic isn’t in the templates or the EHR flags or even the Chunk, Check, Change method. It’s in the *glance*. The way a provider looks at you when they say, ‘I know this is scary.’ Not ‘I’m sorry,’ not ‘Here’s a handout,’ not ‘The FDA says it’s safe.’ Just... a look. Like they see you. Like you’re not a chart, not a code, not a revenue stream. I’ve had providers who handed me a new pill like it was a spare key to a car I didn’t own. And I’ve had one who sat on the edge of the exam table, held my hand, and said, ‘I don’t know when your old one’s coming back. But I know you. And I’ll find you a bridge.’ That’s the drug that saved me. Not the pill. Not the protocol. The human. So yes - use the checklist. But never forget the glance.
Also - I’m 52. I’ve been on 17 different blood pressure meds since 2010. I’ve memorized the color, shape, and smell of each one. When they change it without telling me? I feel like someone swapped my favorite sweater for a plastic bag. That’s not confusion. That’s erasure.
Aaron Bales
1 January 2026Simple fix: Every provider gets a printed one-pager for the top 20 shortage drugs. Keep it in the exam room. Update quarterly. Use the CDC’s plain language. Train every staff member to say the same thing. Done. No EHR changes needed. No extra time. Just consistency.
Lawver Stanton
3 January 2026Let’s be real - this whole article reads like a PowerPoint deck written by a hospital admin who’s never held a stethoscope and whose last patient interaction was a Zoom call with their dog in the background
They talk about ‘structured communication plans’ like it’s some grand innovation
Meanwhile, I’ve been in clinics where the nurse just yells down the hall, ‘Hey, Brenda, Mr. Jenkins is here for his heart pills - they’re out again, right?’
And Brenda yells back, ‘Yeah, try the blue one - it’s cheaper’
And Mr. Jenkins walks out with a new pill and zero context
And now we’re supposed to be impressed because Mayo Clinic has a *system* that takes two minutes?
Two minutes? That’s the bar now?
What about the 80% of clinics that don’t even have an EHR that doesn’t crash every time you try to print a form?
And the ‘dignity’ of patients? The ‘trust’? Please. We’re not fixing communication - we’re just making the paperwork prettier
And don’t even get me started on the ‘cancer specialist’ at Sloan Kettering
That’s not innovation - that’s a luxury we can’t afford
Meanwhile, my aunt in Ohio got switched to a generic and had a seizure because no one told her the new one had a different release profile
And the doctor said, ‘It’s the same active ingredient’
Well duh - but my aunt’s body isn’t a chemistry textbook
So yeah - great article. Now go fix the system that lets this happen in the first place
Not the handouts
Sara Stinnett
4 January 2026There’s a deeper philosophical crisis here - and no one is naming it.
Medicine has been commodified to the point where the patient is no longer a subject, but a data point in a cost-benefit analysis.
The drug shortage is merely the symptom - the disease is the abandonment of the covenant between healer and healed.
We have replaced narrative with protocol, presence with performance metrics, and compassion with compliance.
When we reduce a human being’s fear of death to a checklist item - ‘Did you confirm understanding?’ - we are not healing.
We are auditing.
And the FDA, the Joint Commission, the CDC - they are not saviors.
They are bureaucrats who mistake procedure for virtue.
The real solution? Abolish the EHR. Fire the consultants. And let doctors sit with patients - without templates, without alerts, without KPIs - and talk.
As if their lives depended on it.
Because they do.
linda permata sari
5 January 2026As someone who grew up in Indonesia where medicine is a luxury and you wait months for a refill - I want to say thank you.
Here, when the medicine is gone, you don’t get a handout.
You get silence.
Or worse - a neighbor who says, ‘My cousin’s friend took this yellow pill and it worked.’
So I get it.
When someone takes the time to explain - even in broken English - it feels like being seen.
And that’s worth more than any protocol.
Also - the ‘side-by-side pill chart’? YES.
In my village, we draw pictures on napkins when we can’t find a translator.
Visuals save lives.
Not jargon.
Urvi Patel
7 January 2026This is such a basic level of care it's embarrassing we need an article to remind us
Of course you tell patients why their drug is gone
Of course you use plain language
Of course you check understanding
Anyone with half a brain knows this
Why are we treating this like a breakthrough?
It's not innovation
It's hygiene
Like washing your hands
Stop patting yourselves on the back
Just do your damn job
Marilyn Ferrera
7 January 2026One thing no one mentions: the emotional labor of the provider.
They’re not just giving information - they’re holding space for fear, grief, and uncertainty.
Every time a drug runs out, the provider becomes a counselor, a translator, a detective, and a cheerleader - all in 10 minutes.
And they’re expected to do it while drowning in charting, prior auths, and insurance calls.
So yes - use the checklist.
But also - give them time.
And pay them for the invisible work.
Because clarity isn’t just for patients.
It’s for the people trying to give it.
Robb Rice
8 January 2026Great article. One small note: the phrase 'supply chain disruption' should be replaced with 'the company ran out' - simpler, more honest, and less corporate.
Also - if you're using 'Chunk, Check, Change' - make sure you're not doing it while looking at your computer screen.
Patients notice.
And they feel like an afterthought.
Eye contact matters more than the script.
Just saying.
Harriet Hollingsworth
10 January 2026Someone needs to tell the FDA that ‘generic’ doesn’t mean ‘identical’
My thyroid med? Switched to generic. I gained 22 pounds. My heart raced. I felt like I was drowning in my own skin.
They said ‘same active ingredient’
But my body didn’t get the memo.
So now I pay $180 a month for the brand because I’m not dying because of a cost-cutting algorithm.
And the provider? They shrugged.
‘It’s supposed to work the same.’
Well, it didn’t.
So don’t tell me about ‘proven alternatives’
Some of us aren’t lab rats.
Deepika D
12 January 2026Let me tell you about my cousin in Delhi - she’s diabetic, works 12-hour shifts cleaning offices, and gets her insulin from a street vendor because the hospital ran out for three months straight.
She doesn’t have an EHR.
She doesn’t have a doctor who texts her.
She has a phone number of a nurse who sometimes answers at 2 a.m.
And guess what? She’s alive.
Because when the medicine ran out, that nurse didn’t send a handout.
She walked 3 miles to the pharmacy, bought an extra vial, and brought it to her.
She didn’t say ‘Chunk, Check, Change.’
She said, ‘Here. I got you.’
That’s care.
Not protocols.
Not templates.
Not even plain language.
Just someone showing up.
So yes - use the checklist.
But don’t forget - the most powerful medicine is still someone who refuses to let you fall.
And if your system doesn’t let you do that?
Then your system is broken.
Not your heart.